Emerging markets in Southeast Asia, Latin America, and Africa offer great growth opportunities for healthcare companies looking to build telehealth apps. However, expanding telehealth in these areas requires different strategies than those used in Western markets, where standard infrastructure and predictable user behavior make implementation easier.
Within emerging markets, the challenge lies in fragmented internet connectivity, various payment systems, inconsistent regulations across borders, and populations with different levels of comfort with digital tools. Successful telehealth apps in these markets need designs that are lightweight and can function on low bandwidth, support for multiple languages with cultural nuances considered, payment options that include everything from cash to mobile wallets, and user-friendly interfaces that cater to varying levels of tech experience.
Intellivon creates telehealth apps that address these specific market needs. The platforms offer offline functionality to keep services available despite connectivity gaps, compliance frameworks that fit different regulatory environments, and localized experiences that connect with diverse user groups.
This blog focuses on how we design, govern, and scale telehealth platforms across emerging markets while managing regulatory risk, operational complexity, and clinical accountability.
What You Need to Know Before Building Telehealth Apps for Emerging Markets
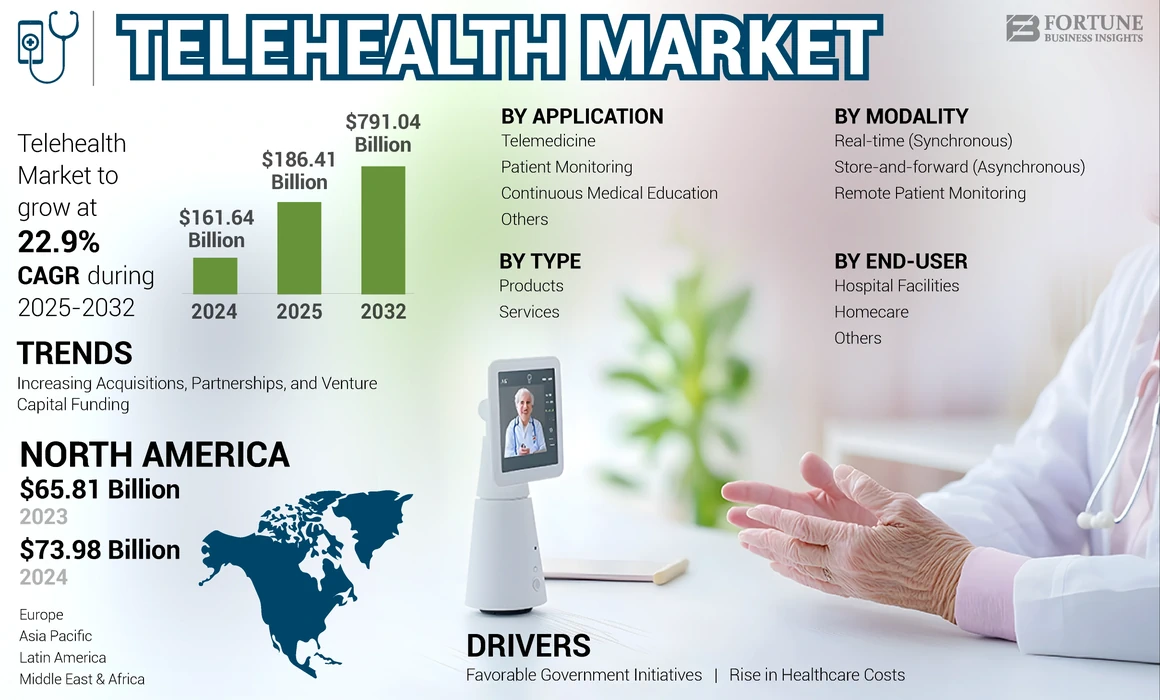
In 2025, the global telehealth market reached a valuation of USD 186.41 billion. The market is expected to expand to USD 219.31 billion in 2026 and accelerate sharply, reaching USD 1,272.81 billion by 2034. This growth reflects a strong 24.60% CAGR over the forecast period. Telehealth in emerging markets is not a convenience layer. It functions as core healthcare infrastructure, designed to extend limited clinical capacity under real operational constraints.
Market Insights:
- Asia-Pacific telehealth to hit USD 105.7 billion by 2030. Here, India alone is projected at USD 9.88 billion by 2026, fueled by eSanjeevani’s 8 crore consultations.
- Rwanda case: Babylon Health delivered 1.2 million consultations since 2016, reaching 30% of adults (2M+ users) via SMS/voice on feature phones despite 1.3 doctors per 10,000 people.
- Latin America’s telehealth is at USD 11.42 billion. At the same time, Africa is growing via NGOs and 5G pilots to bridge rural gaps where 64% live remotely.
Why To Invest In Emerging Markets
These environments present a strong investment case for telehealth because structural gaps continue to widen. Doctor availability remains low at 1.3–2 per 10,000 people, compared to the global average of 15.1.
At the same time, nearly 64% of populations in markets like India and Rwanda live in rural areas, where physical infrastructure expansion remains slow. In addition, government-backed programs such as India’s eSanjeevani, with 8 crore consultations, and Rwanda’s insurance-led digital coverage reaching 90% of citizens, reduce adoption risk and enable enterprise partnerships.
Because per-capita income remains low, cost-efficient telehealth models focused on chronic care deliver measurable ROI by reducing system-level healthcare gaps.
Defining “Emerging Markets” in the Telehealth Context
In a telehealth context, emerging markets describe healthcare systems under structural strain. Population growth, urban–rural divides, and clinician shortages create persistent access gaps. At the same time, mobile adoption and digital payments scale faster than hospitals or specialist networks.
Under these constraints, these markets sit in transition. Care demand rises quickly, but physical expansion moves slowly. At the same time, governments, insurers, and enterprises respond by prioritizing digital care models that extend reach without heavy capital investment. This combination makes telehealth a system-level necessity rather than an optional channel.
Key characteristics usually include:
- Limited doctor and specialist density
- High rural or semi-urban populations
- Mobile-first access patterns
- Fragmented or evolving regulation
- Strong government or payer involvement
What Telehealth Apps Mean in Emerging Markets
In emerging markets, telehealth functions as a healthcare access and capacity multiplier rather than a convenience channel. Platforms are designed to extend limited clinical resources through low-bandwidth care, assisted workflows, and protocol-driven escalation. At the same time, success depends on reliability, governance, and integration with public health and payer systems, not feature density.
Telehealth apps in emerging markets function differently from those in mature healthcare systems. They do not exist primarily as convenience tools. Instead, they operate as access and capacity multipliers within constrained environments.
These platforms focus on enabling care where infrastructure is thin. They prioritize remote triage, follow-ups, and guided escalation rather than full digital replacement of hospitals. As a result, design choices favor reliability over sophistication and reach over feature depth.
In practice, telehealth apps in emerging markets:
- Support voice, SMS, and low-bandwidth interactions
- Embed structured intake and protocol-driven workflows
- Enable task shifting across nurses and community workers
- Integrate with public health programs and insurers
- Emphasize scale, cost control, and clinical governance
Because affordability and trust shape adoption, these apps align closely with national health priorities and enterprise-led care delivery models. They succeed when built as long-term operating systems rather than standalone consumer products.
Core Healthcare Problems Telehealth Solves in Emerging Economies
Telehealth addresses enterprise healthcare constraints by decoupling care delivery from physical capacity. It extends clinician reach, lowers operational costs, improves continuity across fragmented systems, and stabilizes workforce load. When designed as infrastructure, telehealth enables sustainable growth without increasing regulatory exposure or compromising clinical governance.
Healthcare enterprises in emerging economies face problems that scale faster than facilities or staff. Demand rises across primary care, chronic conditions, and preventive services. However, physical infrastructure grows slowly and unevenly.
As a result, operating models strain under volume, cost, and workforce limitations. Telehealth addresses these constraints by redesigning how care enters and moves through enterprise systems.
1. Limited Clinical Capacity Restricts Enterprise Growth
Enterprises struggle to scale when clinician availability remains fixed. Doctor shortages limit appointment throughput and delay care delivery. Therefore, growth often increases wait times instead of outcomes. Telehealth platforms extend clinician reach through remote triage, follow-ups, and escalation pathways.
As a result, enterprises increase service capacity without hiring at the same pace. This shift protects quality while enabling expansion across regions.
2. High Cost-to-Serve Undermines Sustainable Operations
In emerging markets, cost sensitivity shapes every decision. Physical clinics, specialist referrals, and hospital-based follow-ups raise per-patient costs quickly. However, many conditions do not require in-person care. Telehealth shifts low-acuity and routine interactions into digital channels.
Consequently, enterprises reduce overhead while maintaining clinical oversight. Cost savings then fund broader coverage and new service lines.
3. Rural and Distributed Populations Limit Care Reach
Enterprises often serve populations spread across rural or semi-urban areas. Building facilities at that scale remains capital-intensive. At the same time, inconsistent connectivity complicates traditional digital care models. Telehealth platforms designed for voice, SMS, and assisted workflows bridge this gap.
Therefore, enterprises extend their reach without waiting for infrastructure maturity. Access expands while operational complexity stays manageable.
4. Fragmented Care Delivery Reduces Outcome Visibility
Emerging-market healthcare systems often operate in silos. Patients move between clinics, labs, pharmacies, and insurers with little coordination. This fragmentation limits enterprise-level insight into outcomes and utilization. Telehealth platforms centralize intake, documentation, and follow-up.
As a result, enterprises gain end-to-end visibility into care journeys. Data then informs capacity planning, risk management, and performance improvement.
5. Workforce Burnout Threatens Service Continuity
Clinicians and frontline staff face high workloads and administrative burdens. Burnout increases attrition and reduces care consistency. Telehealth platforms automate documentation, triage, and routing tasks. Therefore, clinical staff focus on judgment-driven work rather than repetitive processes.
This balance improves retention while stabilizing service delivery.
For healthcare enterprises, telehealth in emerging economies solves problems that physical expansion cannot. It increases clinical capacity, controls costs, extends reach, and restores operational visibility.
More importantly, it creates a foundation for sustainable growth under real-world constraints. When designed correctly, telehealth shifts enterprises from reactive delivery to scalable, outcome-driven healthcare systems.
90%+ Care Demand Cannot Be Met With Just 1–2 Doctors per 10,000
When countries operate with only 1–2 doctors per 10,000 people, telehealth becomes a structural requirement rather than an optional channel.
Healthcare capacity in many emerging markets is constrained at the foundation level. As populations grow and chronic conditions rise, this imbalance widens each year. Therefore, traditional hospital expansion alone cannot close the gap. Remote-first telehealth emerges as the only scalable way to extend clinical reach without overloading limited medical staff.
1. Physician Scarcity Forces Care Delivery to Decouple From Physical Presence
In systems with extreme doctor shortages, every in-person visit carries an opportunity cost. Clinicians spend time on low-risk follow-ups instead of high-acuity cases. As a result, queues grow while outcomes stagnate.
Telehealth platforms allow care delivery to separate triage from escalation. Doctors intervene where judgment matters most, while technology absorbs routine demand.
This shift does not replace clinicians. Instead, it multiplies their effective capacity across geographies and populations.
2. Remote Triage Reduces Load Without Compromising Clinical Control
Remote-first triage changes how care enters the system. Structured digital intake captures symptoms, history, and risk indicators before a clinician engages. Therefore, consultations start with context rather than discovery. In Rwanda, this model enabled over 1.2 million remote consultations, freeing providers from unnecessary in-person visits.
Escalation remains tightly governed. High-risk cases move to physical facilities, while low-risk interactions resolve remotely. This balance protects clinical quality while preserving scarce physician time.
3. Task Shifting Works Only When Telehealth Platforms Are Designed for It
Emerging markets rely heavily on nurses, community health workers, and mid-level practitioners. However, task shifting fails without proper clinical guardrails. Telehealth platforms enforce protocols, decision trees, and escalation thresholds consistently. As a result, non-physician staff operate within safe boundaries.
Doctors maintain oversight without constant involvement. This structure increases throughput while reducing burnout and error risk.
4. Remote-First Models Align With Rural and Low-Infrastructure Realities
In many emerging economies, over 60% of the population lives in rural areas with limited healthcare facilities. Building hospitals at that scale remains economically unrealistic. However, voice- and SMS-based telehealth works even without broadband connectivity. Therefore, access expands without waiting for infrastructure maturity.
This approach meets populations where they already are. Adoption follows naturally when care fits daily realities.
When physician density drops to 1–2 per 10,000 people, healthcare systems face a hard constraint, not a temporary shortage. Telehealth resolves this constraint by redesigning how care enters, flows through, and escalates within the system. Remote-first models protect clinicians, expand reach, and stabilize outcomes.
Telehealth Adoption Models That Actually Work
Given the structural constraints discussed earlier, which include clinician scarcity, rural access gaps, and cost sensitivity, telehealth adoption in emerging markets depends heavily on how care is funded, governed, and delivered.
Telehealth adoption in emerging markets succeeds when platforms align with funding, governance, and delivery structures. Employer-led, hospital-integrated, insurer-backed, and government-sponsored models scale more reliably than direct-to-consumer approaches alone. At the same time, enterprises achieve resilience by combining adoption paths to distribute financial, regulatory, and operational risk.
These apps in emerging economies succeed when platforms align with how care is funded, governed, and delivered, rather than relying on a single go-to-market model. As a result, models that scale well in mature systems often underperform when copied directly. Therefore, choosing the right adoption model becomes a strategic decision, not an operational detail.
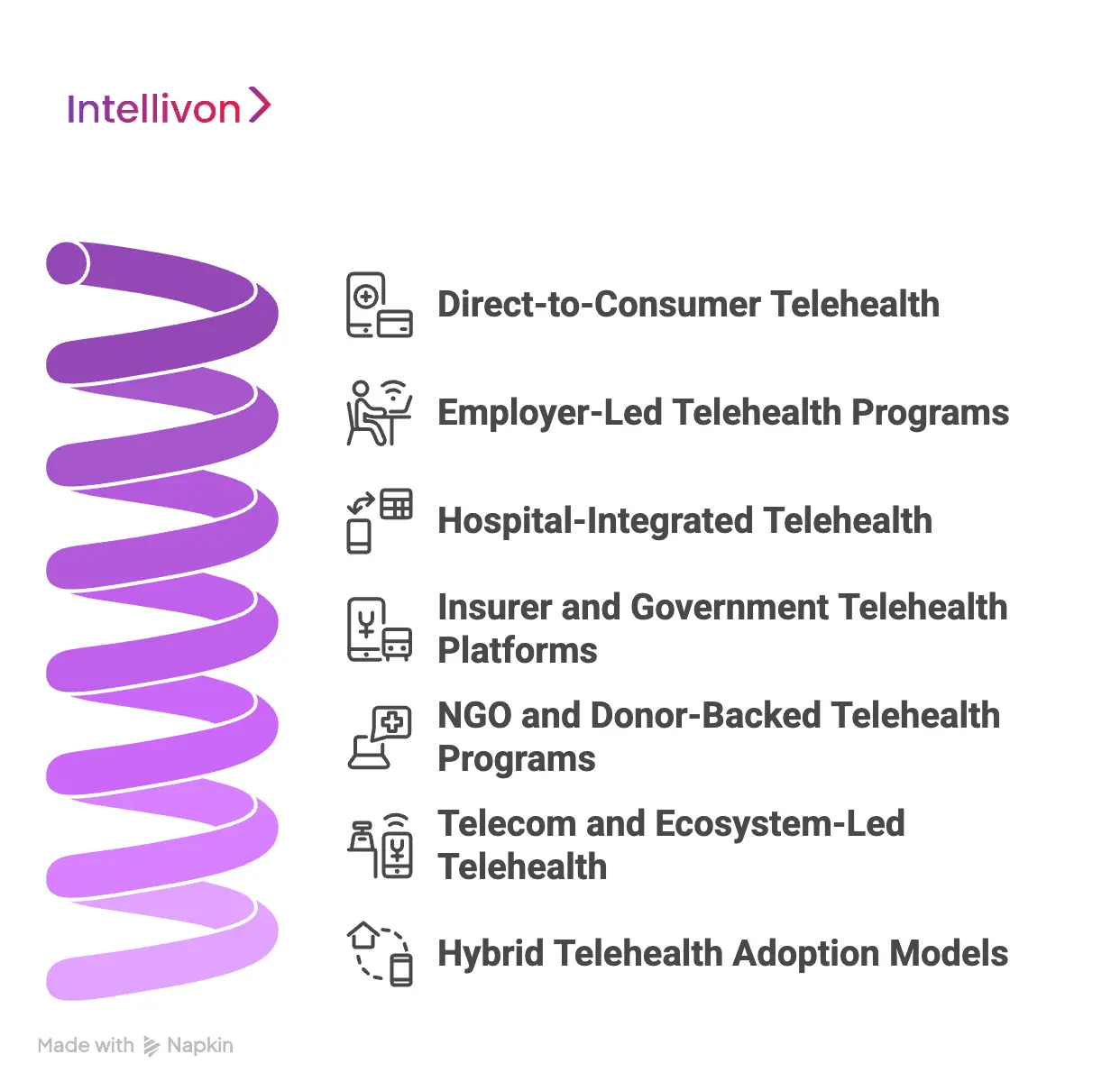
1. Direct-to-Consumer Telehealth
Direct-to-consumer telehealth enables fast entry into new markets. Patients self-pay, onboarding remains simple, and early adoption grows quickly. However, price sensitivity shapes usage patterns and limits repeat engagement.
As a result, churn increases once acute needs resolve. Enterprises often use this model to test demand, launch niche services, or support urban users. At scale, however, DTC rarely sustains enterprise-grade economics on its own.
2. Employer-Led Telehealth Programs
Employer-led telehealth embeds care into workforce benefit structures. As a result, utilization remains more consistent and less dependent on individual willingness to pay. Enterprises subsidize access, which reduces friction and supports higher retention.
Therefore, this model works well for chronic care, mental health, and preventive services. Many platforms rely on employer programs to stabilize revenue while expanding reach across regions.
3. Hospital-Integrated Telehealth
Hospital-integrated telehealth leverages existing clinical trust and governance. Platforms align with hospital workflows, which improves care continuity and regulatory compliance. However, deployment cycles move slowly due to procurement processes and legacy systems.
Despite this, hospital integration remains essential for regulated services and complex treatment pathways. Enterprises often accept longer timelines in exchange for credibility and long-term clinical alignment.
4. Insurer and Government Telehealth Platforms
Insurer- and government-sponsored telehealth focuses on population-level access. These platforms scale quickly through coverage mandates and policy support. Therefore, adoption risk decreases significantly. However, compliance requirements increase, and margins remain tight.
Enterprises succeed here by designing platforms for auditability, reporting, and long-term contracts. This model prioritizes stability and scale over rapid monetization.
In an insurer-led telehealth program, the platform was structured around remote triage, follow-ups, and controlled escalation to in-person care. Integration with claims and care management systems improved utilization visibility while maintaining cost controls. The model supported population-scale access without disrupting existing provider networks.
5. NGO and Donor-Backed Telehealth Programs
NGO-backed telehealth programs often operate in underserved or remote regions. These initiatives focus on maternal health, infectious diseases, and mental health access. As a result, platforms function under real-world constraints from the outset.
While direct revenue remains limited, enterprises gain operational insight and proof of impact. Over time, many of these programs transition into public or insurer-backed models.
6. Telecom and Ecosystem-Led Telehealth
Telecom-led telehealth uses existing mobile infrastructure to extend reach. By supporting voice, SMS, and subsidized data access, platforms overcome connectivity barriers. Therefore, adoption scales without requiring smartphones or high bandwidth.
Enterprises partner with telecom providers to solve distribution challenges. This model works well for triage, follow-ups, and health awareness programs.
7. Hybrid Telehealth Adoption Models
Hybrid adoption models combine multiple funding and delivery paths. Platforms often blend government scale, employer stability, and selective consumer access. As a result, risk is distributed across channels.
Enterprises gain resilience against policy shifts and market volatility. This approach reflects how telehealth platforms sustain growth across diverse emerging markets.
Telehealth adoption in emerging economies rewards alignment over simplicity. No single model fits every market or use case. Instead, enterprises succeed by selecting and combining adoption paths that match funding structures and care realities. When designed with realism, telehealth platforms move from pilots to infrastructure.
Key Design Principles for Telehealth Apps in Emerging Markets
Because emerging-market telehealth must operate under the constraints outlined earlier, design decisions prioritize reliability, access, and trust over feature sophistication.
Effective telehealth design in emerging markets prioritizes reliability over sophistication. Here, low-bandwidth performance, offline-first data capture, device-agnostic interfaces, multilingual support, and trust cues are essential. These principles reduce drop-offs, stabilize clinical workflows, and ensure platforms remain usable under inconsistent connectivity and infrastructure constraints.
Telehealth apps succeed in emerging markets when design prioritizes reliability, access, and trust over feature richness and bandwidth-heavy experiences. Therefore, enterprises cannot rely on design patterns borrowed from mature healthcare systems. Instead, platforms must operate reliably under imperfect conditions. These principles separate pilots that struggle from systems that scale sustainably.
1. Low-Bandwidth User Experience
Connectivity remains inconsistent across many regions. As a result, telehealth apps must function well even when networks degrade. Adaptive video, audio-only modes, and asynchronous consultations reduce dependency on stable broadband. Therefore, care delivery continues without interruption.
Enterprises benefit because service reliability improves across rural and semi-urban populations. This consistency directly impacts adoption and retention.
In a low-bandwidth rural deployment, the telehealth platform relied on audio consultations, asynchronous follow-ups, and delayed data synchronization. Device constraints and intermittent connectivity shaped every design decision. Reliability, rather than feature depth, determined sustained adoption across field clinicians and patients.
2. Offline-First Data Capture
Many care interactions occur where connectivity drops unexpectedly. Therefore, platforms must capture clinical data offline and sync later without loss. Forms, notes, and vitals should be stored locally until networks recover. This approach prevents workflow disruption.
For enterprises, offline-first design protects data integrity. It also ensures clinicians and field staff remain productive throughout the day.
3. Device-Agnostic Application Design
Emerging markets rely heavily on low-end Android devices. Screen sizes vary, memory is limited, and processing power remains modest. Therefore, telehealth apps must remain lightweight and responsive. Heavy animations and large downloads slow adoption.
Enterprises that design for device diversity reduce support burden. As a result, platforms reach wider populations without fragmentation.
4. Multilingual and Low-Literacy Interfaces
Language diversity shapes adoption more than features. Many users are first-time digital health adopters. Therefore, interfaces must support local languages, simple prompts, and visual guidance. Clear icons and step-by-step flows reduce confusion.
Enterprises gain higher completion rates and fewer support requests. This clarity improves operational efficiency and patient confidence.
5. Trust-Building User Experience
Trust determines whether users return for care. Clear doctor profiles, verified credentials, and transparent consultation steps build confidence. Therefore, users feel comfortable sharing health information. Consistent branding and secure access reinforce credibility.
For enterprises, trust reduces churn and complaint rates. Over time, it strengthens the platform’s reputation across communities.
In emerging markets, design choices carry operational consequences. Enterprises that design with these principles build platforms that endure real-world constraints. As a result, telehealth becomes a dependable infrastructure rather than a fragile digital layer.
Role of Public–Private Partnerships (PPPs) in Telehealth Expansion
Public–private partnerships accelerate telehealth expansion in emerging markets by combining government scale, private execution capability, and shared accountability for outcomes.
At the same time, enterprises bring execution speed, technology depth, and operational discipline. Therefore, public–private partnerships become the most practical path to scale. PPPs reduce adoption risk while aligning telehealth with national healthcare priorities.
In a government-backed telehealth rollout across rural regions, platform design prioritized voice-first access, offline data capture, and protocol-driven escalation. Regulatory reporting and audit trails were embedded from the start to support public accountability. This approach enabled scale without increasing clinical or compliance risk.
1. Governments Provide Scale and Legitimacy
Public institutions anchor trust in many emerging economies. When governments endorse telehealth platforms, adoption accelerates across populations. As a result, patient confidence improves, and provider participation increases. Policy backing also simplifies regulatory alignment and reimbursement flows.
For enterprises, this legitimacy lowers go-to-market friction. Platforms enter the system as infrastructure, not experiments.
2. Enterprises Drive Execution and Innovation
While governments define scope, enterprises execute delivery. Private partners design platforms, integrate systems, and manage day-to-day operations. Therefore, telehealth programs move faster than purely public initiatives. Iteration cycles remain short, and technology evolves with usage patterns.
This division of responsibility allows innovation without sacrificing oversight. It also keeps platforms responsive to real-world constraints.
3. PPPs Enable Sustainable Funding Models
Telehealth expansion requires predictable funding. PPPs blend public budgets, insurer participation, and enterprise investment. As a result, platforms avoid reliance on volatile consumer spending.
Cost-sharing structures distribute financial risk across stakeholders. For enterprises, this stability supports long-term planning. It also improves confidence in scaling beyond pilot phases.
4. Standardization Improves System-Wide Outcomes
Fragmented digital health efforts dilute impact. PPPs encourage standard protocols, shared data models, and interoperable systems. Therefore, telehealth integrates more cleanly with public health infrastructure. Reporting and monitoring improve at a national level.
Enterprises benefit from clearer requirements and repeatable deployment models. Over time, delivery becomes more efficient.
5. Accountability Shifts From Access to Outcomes
Early telehealth programs often focus only on access. PPPs shift attention toward outcomes, efficiency, and utilization. At the same time, governments track performance, while enterprises optimize delivery.
As a result, telehealth moves from volume-driven adoption to value-driven care. This alignment strengthens program durability. It also creates a stronger case for continued investment.
Public–private partnerships transform telehealth from isolated platforms into a national care infrastructure. Governments contribute scale, trust, and policy alignment. For emerging markets, PPPs are the mechanism that turns telehealth ambition into sustained impact.
AI’s Role in Scaling Telehealth in Emerging Markets
Once core access and workflow constraints are addressed, AI becomes the primary lever for scaling telehealth without increasing clinical or operational risk.
AI enables telehealth platforms to scale safely by improving triage accuracy, care routing, task-shifting support, and early risk detection. However, scale is sustainable only when AI operates within defined decision boundaries, includes human oversight, and maintains auditability. Governed AI increases capacity without eroding clinical or regulatory trust.
Therefore, telehealth platforms cannot rely on human workflows alone. AI becomes essential, not as a replacement for clinicians, but as a force multiplier. When applied correctly, it allows enterprises to expand reach while preserving safety and governance.
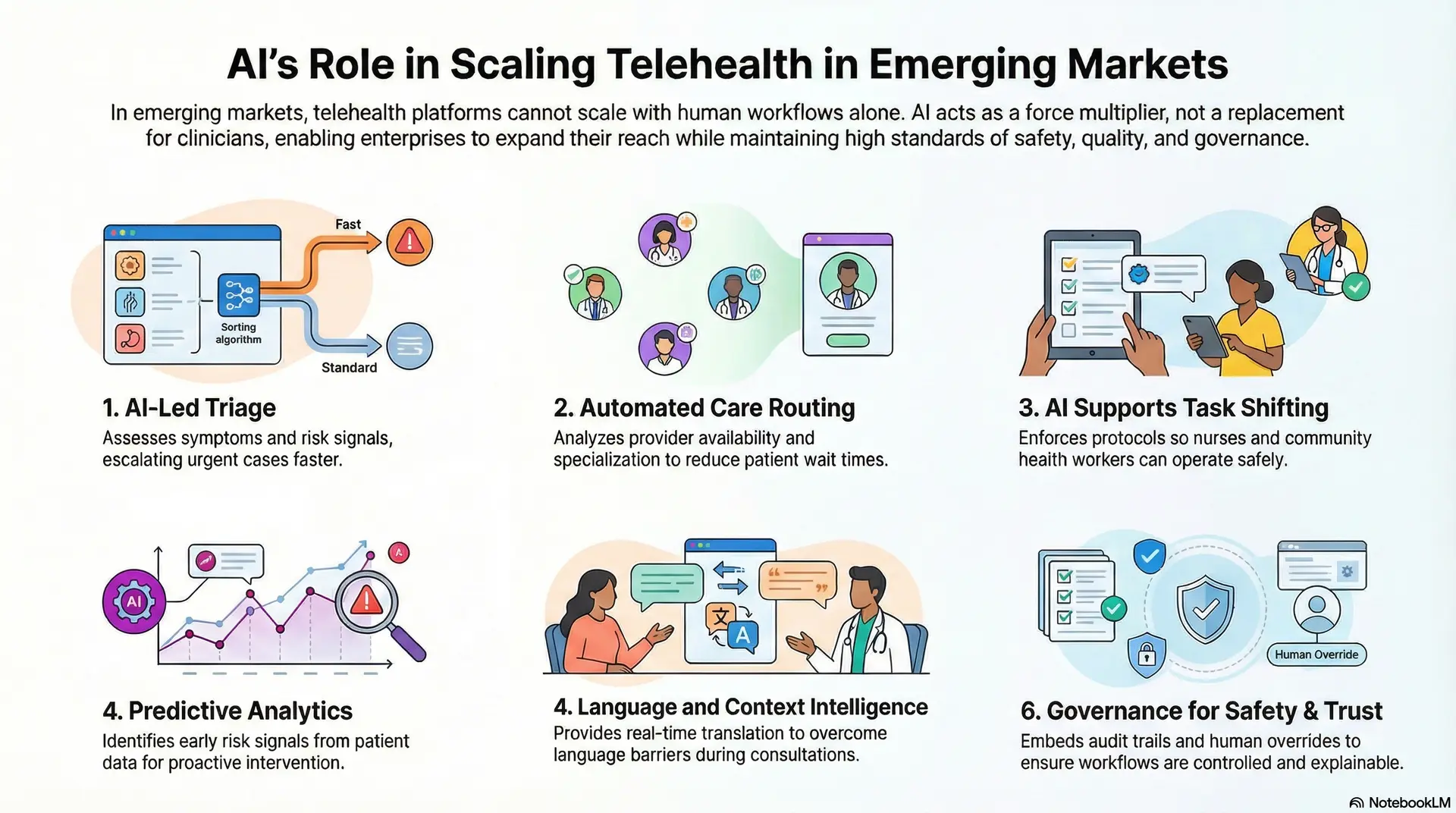
1. AI-Led Triage
AI-driven triage systems assess symptoms, history, and risk signals before a clinician engages. As a result, low-risk cases resolve earlier while urgent cases escalate faster.
This separation improves throughput without compromising care standards. Therefore, clinicians spend time where judgment matters most.
For enterprises, this directly increases capacity. It also stabilizes service levels as demand fluctuates across regions.
2. Automated Care Routing
Telehealth platforms often fail when cases route inefficiently. AI models analyze availability, specialization, and workload in real time. As a result, patients reach the right provider faster. Wait times drop, and utilization improves.
This routing intelligence reduces manual coordination. Consequently, enterprises operate leaner care networks at scale.
3. AI Supports Task Shifting
Emerging markets rely heavily on nurses and community health workers. However, task shifting requires strict boundaries. AI decision support enforces protocols, flags risks, and triggers escalation when thresholds break. Therefore, non-physician staff operate safely within defined limits.
Enterprises benefit from expanded delivery capacity. At the same time, clinical accountability remains intact.
4. Language and Context Intelligence
Language diversity limits adoption in many regions. AI-powered translation and transcription reduce friction during consultations. As a result, providers and patients communicate clearly without shared language fluency. Context-aware prompts also improve data capture quality.
This capability allows enterprises to scale across regions without duplicating clinical teams. It also improves documentation consistency.
5. Predictive Analytics
AI models analyze longitudinal data to identify early risk signals. Therefore, telehealth platforms intervene before conditions escalate. Chronic care programs benefit the most from this approach. Hospital visits reduce, and outcomes improve over time.
For enterprises, predictive insights support cost control. They also strengthen the business case for preventive and continuous care programs.
6. Governance Keeps AI Safe and Trusted
AI in telehealth must remain controlled and explainable. Enterprises embed audit trails, human override mechanisms, and performance monitoring. As a result, regulators and clinicians trust AI-supported workflows.
Transparency prevents misuse and erosion of confidence. Without governance, scale introduces risk. With governance, AI enables safe expansion.
AI determines whether telehealth platforms stall or scale in emerging markets. When used to support triage, routing, task shifting, and prevention, it amplifies human capacity without eroding trust. For enterprises, AI is not a feature layer. It is the engine that makes large-scale, affordable telehealth operationally viable. Used responsibly, it turns constraint into leverage.
Technology Architecture Of Telehealth Apps For Emerging Markets
To manage the operational and regulatory complexity described earlier, telehealth platforms in emerging markets must be built on layered, modular architectures.
Enterprise telehealth platforms scale reliably when built on layered architectures that separate access, workflows, intelligence, data, compliance, and infrastructure concerns. This structure isolates regional risk, supports phased expansion, and allows each layer to evolve independently without destabilizing clinical operations or regulatory controls.
Telehealth platforms in emerging markets scale reliably when built on layered architectures that separate access, intelligence, compliance, and infrastructure concerns.
Enterprises require layered architectures that isolate risk while allowing selective scale. Each layer serves a specific function, yet integrates cleanly with the rest.
1. Access & Experience Layer
This layer manages how patients, providers, and administrators interact with the platform. It must remain lightweight, resilient, and tolerant of low bandwidth. Therefore, experiences degrade gracefully rather than fail outright. Accessibility and trust cues originate here.
Technology stack
- Android (low-end optimized)
- Progressive Web Apps (PWA)
- React Native / Flutter
- WebRTC (adaptive video)
- SIP / VoIP
- SMS / USSD gateways
2. Workflow & Orchestration Layer
This layer controls how care flows through the system. It governs triage, scheduling, escalation, and task routing. Therefore, it ensures consistency regardless of the entry point. Business rules live here, not in the interface.
Technology stack
- BPMN engines
- Workflow orchestration services
- Rules engines
- Event-driven architectures
- Message queues
3. Clinical Intelligence & AI Layer
This layer augments human decision-making. It processes intake data, flags risks, and supports routing decisions. Therefore, it reduces clinician load while preserving judgment boundaries. Explainability and override controls remain essential.
Technology stack
- Machine learning models
- Natural language processing
- Clinical decision support systems
- Risk scoring engines
- Model monitoring tools
4. Data Management & Interoperability Layer
This layer handles clinical, operational, and engagement data. It ensures consistency across fragmented systems. Therefore, it supports continuity of care and reporting. Standards compliance remains critical.
Technology stack
- HL7 / FHIR APIs
- Data normalization services
- ETL pipelines
- API gateways
- Master data management tools
5. Security, Privacy & Compliance Layer
This layer enforces regulatory and ethical controls. It governs identity, access, consent, and auditability. Therefore, it protects patient trust and enterprise liability. Controls operate continuously, not at checkpoints.
Technology stack
- Identity and access management (IAM)
- Role-based access control (RBAC)
- Consent management systems
- Encryption services
- Audit logging tools
6. Infrastructure & Scalability Layer
This layer supports reliability and growth. It absorbs traffic spikes and regional expansion. Therefore, it ensures uptime without overprovisioning. Resilience matters more than raw performance.
Technology stack
- Cloud infrastructure (AWS, Azure, GCP)
- Containerization (Docker)
- Kubernetes
- Auto-scaling groups
- Edge caching services
Layered architecture determines whether telehealth platforms survive real-world conditions. Each layer evolves independently without destabilizing the whole. In emerging markets, this architectural discipline turns complexity into controlled scale.
Compliance and Regulatory Requirements For Telehealth Apps
As highlighted throughout this guide, regulatory fragmentation is one of the defining challenges of telehealth in emerging markets.
Telehealth compliance in emerging markets requires country-aware governance rather than uniform policy enforcement. Platforms must manage clinician licensing, prescribing rules, consent standards, and data residency at the workflow level. Embedding these controls into system design reduces regulatory exposure and supports scalable, multi-country deployment.
Telehealth compliance in emerging markets requires flexible, country-aware governance models that balance patient safety, data protection, and evolving regulatory frameworks.
Instead, telehealth platforms must adapt to fragmented legal, clinical, and data governance environments. A compliance-by-design approach protects growth while reducing regulatory exposure.
1. Fragmented Regulations Across Countries
Unlike mature markets, emerging economies rarely operate under unified telehealth laws. Each country defines its own rules for licensing, prescribing, and care delivery. As a result, platforms must manage country-specific compliance layers. What works in one market may fail in another.
Enterprises succeed by isolating regulatory logic. This approach allows expansion without rewriting core systems.
2. Medical Licensing and Scope of Practice
Clinician licensing remains a major constraint. Many countries restrict cross-border consultations or define narrow telemedicine scopes. Therefore, telehealth apps must enforce provider eligibility at a local level. Automated checks prevent unlicensed practice.
This control protects enterprises from legal risk. It also maintains clinical credibility with regulators.
3. Patient Data Protection and Privacy
Data privacy laws vary widely across emerging markets. Some regions mandate local data storage, while others lack formal enforcement. However, patient trust still depends on strong safeguards. Therefore, platforms must enforce encryption, consent, and access controls consistently.
Enterprises that exceed minimum requirements reduce long-term exposure. Strong privacy practices also ease future regulatory tightening.
4. Consent and Patient Rights Management
In emerging markets, informed consent often lacks standardization. Literacy levels, language diversity, and cultural norms complicate consent workflows. Therefore, telehealth platforms must capture consent clearly and audibly.
Digital consent records must remain auditable. This transparency protects enterprises during disputes. It also improves patient confidence.
5. Prescription and Medication Rules
Tele-prescribing rules differ sharply across regions. Some countries allow digital prescriptions, while others restrict controlled substances. As a result, telehealth apps must enforce medication rules dynamically. Automated checks reduce misuse.
Enterprises that embed these controls avoid compliance breaches. They also build trust with pharmacies and regulators.
6. Auditability and Reporting Obligations
Governments and insurers increasingly require performance visibility. Telehealth platforms must support audits, usage reporting, and clinical outcomes tracking. Therefore, logging and reporting cannot remain afterthoughts.
Enterprises that prepare early reduce friction during inspections. This readiness also supports PPP and insurer partnerships.
Compliance in emerging markets is complex, dynamic, and unavoidable. Telehealth platforms must navigate fragmented regulations, licensing limits, and evolving data laws. In emerging markets, regulatory readiness determines long-term viability.
How We Build Telehealth Apps For Emerging Markets
Building telehealth for emerging markets requires execution discipline over speed. Successful platforms align care models, regulatory constraints, architecture, and AI governance early. Consequently, a structured build approach reduces uncertainty, enables controlled scaling, and ensures telehealth systems remain stable as programs expand across regions and populations.
Intellivon approaches telehealth as a healthcare infrastructure, not a feature layer. Each step in the build process focuses on reducing uncertainty while enabling controlled scale.

Step 1: Define the Care Model and Use Cases
Every build starts by defining how care should flow through the system. Priority conditions, target populations, and expected outcomes are clarified early. As a result, the platform avoids generic feature sets that dilute impact. Care pathways define what happens remotely and what requires escalation.
This step also clarifies who delivers care and where accountability sits. Therefore, business, clinical, and operational goals stay aligned from the outset.
Step 2: Translate Regulations Into Platform Controls
Regulatory requirements differ widely across emerging markets. Licensing rules, prescribing limits, and consent standards vary by country. Therefore, these constraints must shape the platform before development begins.
Rules translate directly into workflows and access controls. This prevents compliance from becoming a manual process. As a result, the platform enforces regulation consistently at scale.
Step 3: Design for Low Bandwidth and Device Diversity
Connectivity varies daily across regions. Devices range from low-end Android phones to shared community terminals. Therefore, experiences must degrade gracefully under weak networks.
Voice, async consults, and lightweight interfaces take priority. Large downloads and heavy animations are avoided. As a result, the platform remains usable even under unstable conditions.
Step 4: Build Modular and Layered Architecture
Scalability requires separation of concerns. The platform is structured into distinct layers for access, workflows, intelligence, data, and infrastructure. Therefore, changes in one layer do not disrupt the entire system.
Regional requirements remain isolated from the core. This structure supports phased expansion across markets. It also simplifies long-term maintenance.
Step 5: Embed AI With Clear Guardrails
AI supports scale when applied with discipline. Triage, routing, and risk scoring automate routine decisions. However, clinical judgment always remains central.
Guardrails define when AI assists and when humans intervene. Explainability and auditability stay intact. Therefore, trust remains high among clinicians and regulators.
Step 6: Integrate With Healthcare and Ecosystem Systems
Telehealth platforms rarely operate alone. Hospitals, labs, pharmacies, insurers, and government systems must connect seamlessly. Therefore, integrations rely on standardized interfaces and clean data flows.
This ensures continuity across the care journey. Reporting and billing also improve. As a result, stakeholders adopt the platform more readily.
Step 7: Pilot, Measure, and Scale Gradually
Large-scale rollouts introduce risk. Therefore, deployment begins with controlled pilots. Early usage reveals operational gaps and workflow friction. Metrics guide refinements before expansion.
At the same time, only stable systems move to broader rollout. As a result, scale occurs without destabilizing service quality.
Telehealth success in emerging markets depends on execution discipline. A structured build process reduces risk while enabling growth. By aligning care models, compliance, design, and architecture early, platforms scale with confidence. This is how Intellivon helps enterprises move from pilots to resilient healthcare infrastructure.
How Telehealth Apps In Emerging Markets Generate Revenue
Telehealth platforms in emerging markets generate revenue by aligning monetization with payers, institutions, and outcomes rather than relying solely on consumer payments.
Revenue models determine whether telehealth platforms survive beyond pilots. In emerging markets, affordability limits direct consumer spending. These models prioritize predictability, scale, and long-term partnerships over one-time transactions.
1. Employer and Enterprise Contracts
Employers increasingly fund healthcare to protect productivity and reduce absenteeism. Telehealth platforms contract directly with enterprises to deliver primary care, mental health, and chronic support. As a result, revenue remains recurring and predictable. Pricing often follows per-employee or per-member-per-month structures.
For platforms, this model reduces churn. It also supports stable forecasting and regional expansion.
2. Insurer and Payer Reimbursements
Insurers adopt telehealth to control claim costs and improve access. Platforms earn revenue through reimbursement agreements tied to consultations, programs, or outcomes. Therefore, volume scales quickly once coverage applies. However, margins remain controlled.
Enterprises that design for payer workflows unlock population-scale revenue. Compliance and reporting then become revenue enablers, not overhead.
3. Government and Public Health Programs
Governments sponsor telehealth to extend access without building facilities. Revenue flows through long-term contracts, tenders, or service fees. As a result, platforms gain scale and policy backing. Payment cycles may move slowly, but contracts provide durability.
This model suits enterprises focused on infrastructure-level deployment rather than rapid monetization.
4. Hospital and Provider Partnerships
Hospitals use telehealth to extend services beyond physical walls. Platforms earn revenue through licensing, integration fees, or shared service models. Therefore, income aligns with provider usage rather than patient volume. This approach works well for specialist access and follow-up care.
Enterprises benefit from clinical credibility. They also embed telehealth deeper into care pathways.
5. Subscription and Program-Based Care
Some platforms bundle services into condition-specific programs. Chronic care, maternal health, and mental wellness often follow subscription pricing. As a result, revenue ties to continuity rather than visits. Engagement improves when care feels ongoing.
This model balances affordability with value. It also supports outcome tracking over time.
6. Diagnostics, Pharmacy, and Ecosystem Revenue
Telehealth platforms often integrate diagnostics and pharmacies. Revenue flows through referrals, commissions, or partnerships. Therefore, platforms monetize the full care journey. This diversification reduces reliance on consultations alone.
Enterprises that orchestrate ecosystems improve margins while enhancing patient convenience.
Telehealth revenue in emerging markets depends on alignment, not volume alone. When monetization matches how healthcare is funded, telehealth becomes a sustainable business, not a temporary solution.
Conclusion
Telehealth in emerging markets is no longer an experiment. It is becoming core healthcare infrastructure. However, success depends on building for constraint, not convenience. Enterprises that align care models, compliance, design, and AI from the start scale faster and with lower risk. They reduce cost pressure while expanding access and outcomes. Most importantly, they create systems that endure policy shifts and infrastructure gaps.
This is where execution matters. With deep experience in enterprise healthcare platforms and AI-led delivery, Intellivon helps organizations turn telehealth ambition into a reliable, scalable impact.
Build Telehealth Platforms for Emerging Markets With Intellivon
At Intellivon, telehealth platforms for emerging markets are built as resilient healthcare operating systems, not lightweight apps adapted from mature markets. Every architectural and delivery decision accounts for infrastructure variability, regulatory fragmentation, and cost sensitivity. The focus stays on long-term viability rather than short-term deployment speed.
Each platform is engineered for real operating conditions where bandwidth fluctuates, devices vary, and care delivery relies on mixed clinical workforces. As platforms scale across regions, populations, or payer models, governance, performance, and compliance remain stable. This approach enables expansion without increasing operational risk or compromising clinical integrity.
Why Partner With Intellivon?
This is a working discussion for enterprise teams evaluating telehealth as a long-term care delivery platform. It is not a sales demo, a generic capability pitch, or a commitment to build. The conversation focuses on feasibility, risk, and execution realities based on your specific operating environment.
- Enterprise-grade telehealth architecture designed to operate under low-bandwidth, device-diverse, and infrastructure-constrained environments
- Proven delivery experience across employer-led, hospital-integrated, insurer-backed, and government-sponsored telehealth models
- Compliance-by-design approach aligned with local regulations, data residency requirements, consent management, and audit readiness
- Secure role-based access control with end-to-end traceability across clinicians, partners, and administrators
- AI-assisted with mandatory human oversight, triage, routing, and preventive workflows.
- Cloud-native, modular infrastructure supporting phased rollout by region, care pathway, or population segment
- Deep interoperability across EHRs, labs, pharmacies, insurers, and public health systems
- Continuous optimization across outcomes, cost efficiency, adoption, and operational performance
Discuss your telehealth platform strategy with us to explore how a telehealth platform can scale sustainably across emerging markets, with Intellivon as your long-term technology, compliance, and execution partner.
FAQs
Q1. What makes telehealth apps successful in emerging markets?
A1. Telehealth apps succeed in emerging markets when they are designed for real operating constraints. Low bandwidth support, offline workflows, and device flexibility matter more than advanced features. In addition, platforms must align with local care delivery models and funding structures. Trust, compliance, and operational reliability ultimately drive sustained adoption, not novelty.
Q2. How much does it cost to build a telehealth app for emerging markets?
A2. Costs depend on platform scope, regions covered, and regulatory complexity. Enterprise-grade telehealth platforms are usually built in phases, starting with core care workflows and compliance controls. As programs scale, costs increase with integrations, AI enablement, and multi-region infrastructure. Therefore, successful enterprises plan for staged investment rather than a single build.
Q3. What regulatory challenges affect telehealth adoption in emerging economies?
A3. Regulatory frameworks vary significantly across countries and often change over time. Common challenges include clinician licensing restrictions, cross-border care limitations, data residency rules, and consent requirements. Telehealth platforms must enforce these rules at the workflow level. As a result, compliance becomes an architectural requirement, not a policy document.
Q4. Can telehealth work effectively in low-connectivity or rural areas?
A4. Yes, when platforms are designed specifically for those conditions. Voice-based care, SMS workflows, and asynchronous consultations reduce dependence on broadband. Offline data capture ensures continuity when networks drop. Therefore, telehealth can reach rural populations without waiting for infrastructure upgrades.
Q5. How does AI help scale telehealth platforms in emerging markets?
A5. AI helps scale telehealth by reducing manual clinical load while preserving safety. It supports triage, case routing, and early risk identification across large populations. At the same time, governance mechanisms keep clinicians in control. When applied responsibly, AI improves efficiency, consistency, and long-term sustainability.