Even though digital access has expanded significantly in recent years, organizations still struggle to turn telemedicine into a consistent, high-impact care channel. Subscriptions sit unused, provider demand fluctuates, and patients hesitate when long-term commitments do not match episodic care needs. At the same time, care consumption patterns are shifting, where patients increasingly seek fast, transactional access for specific concerns. This shift has exposed a gap between how virtual care platforms are monetized and how care is actually delivered.
The pay-per-visit telemedicine platform model addresses this gap by treating virtual care as an on-demand service rather than a recurring obligation. Craft has helped accelerate this shift by designing its platform around visit-based access with real-time provider availability, not long-term user lock-in.
At Intellivon, we have worked closely with healthcare enterprises building regulated digital care platforms that must balance speed, compliance, and scale. That experience shapes how we evaluate models like Craft, beyond surface-level features. In this blog, we break down how to build a pay-per-visit telemedicine platform like Craft from the ground up.
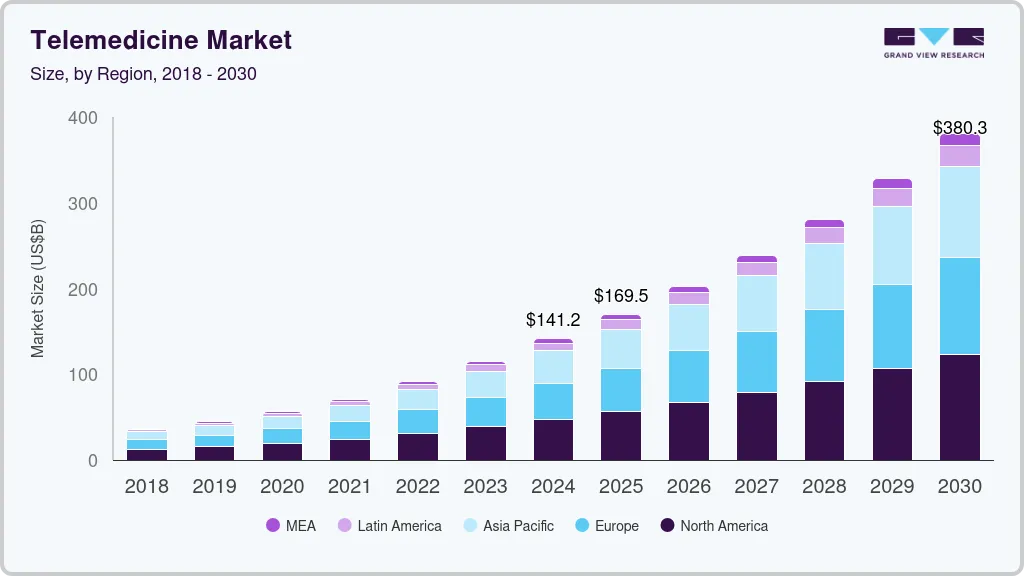
Key Takeaways of the Global Telemedicine Market
According to Grand View Research, the global telemedicine market reached an estimated value of USD 141.19 billion in 2024 and is expected to expand to USD 380.33 billion by 2030, reflecting a 17.55% CAGR between 2025 and 2030.
This growth is being driven by consolidation across healthcare ecosystems, deeper partnerships between providers and technology firms, and a shift toward consumer-driven care experiences.
Market Insights:
- Pricing Benchmarks: One-time virtual consultations typically fall between USD 40 and USD 90 per visit. Major urgent care platforms often price sessions in the mid-USD 40 range for uninsured encounters.
- Delivery Model Share: On-demand web and mobile consultations dominate telemedicine usage, accounting for nearly four-fifths of total revenue due to faster access and lower setup friction.
- Cost Savings: Real-time video consultations can reduce per-visit costs by approximately USD 19 to USD 121 compared to in-person care, primarily by eliminating travel, wait times, and productivity loss.
- Reimbursement Landscape: Pay-per-visit telemedicine services are commonly reimbursed through fee-for-service CPT billing, with Medicare and commercial payers continuing to expand eligible virtual care codes and facility fee coverage.
- Growth Drivers: Wider broadband and 5G availability, rising chronic disease prevalence, demand for episodic care, and payer-led cost containment strategies are accelerating on-demand telemedicine adoption.
- Core Use Cases: This model is well-suited for urgent care triage, behavioral health consultations, and primary care follow-ups, often serving as a low-friction digital entry point for episodic clinical needs.
What Is The Pay-Per-Visit Telemedicine Platform Craft?
A pay-per-visit telemedicine platform like Craft enables patients to access virtual care on demand, pay once per consult, and exit without subscription commitments.
What the Platform Is
Craft is built around immediate clinical access without ongoing financial obligations. Patients use the platform when a need arises, complete a virtual visit, and pay only for that encounter. There are no monthly plans, bundled contracts, or usage thresholds to manage.
This structure makes the platform especially effective for short, episodic care needs. Urgent concerns, routine follow-ups, and first-time consultations fit naturally into this model. For enterprises, it simplifies pricing while expanding digital access across broader patient populations.
How the Craft-Style Model Works
The workflow is intentionally simple. Patients begin by selecting the type of visit they need, such as urgent care, primary care, or behavioral support. Based on that selection, the platform surfaces available clinicians in real time or allows scheduled access when appropriate.
Once a provider is chosen, the patient completes a one-time payment before the consultation begins. After the visit, clinical notes, prescriptions, and care summaries are securely delivered through the platform. This closed-loop flow reduces drop-offs and improves visit completion rates.
Who This Model Is Best Suited For
This model works well for health systems looking to extend access without overhauling existing care delivery. It supports clinics managing after-hours demand or sudden patient surges without adding physical capacity.
Employers and insurers also benefit by offering episodic virtual care as a flexible benefit. In these settings, pay-per-visit access provides cost control while maintaining a positive care experience for members.
How It Works
A Craft-style pay-per-visit workflow moves patients from visit selection to payment, consultation, documentation, and follow-up in one secure, closed-loop flow.
1. Patient Enters the Platform
They choose immediate care or schedule a visit. The platform confirms location, eligibility, and basic access requirements.
2. Visit Type is Selected
The patient picks a service line, such as urgent care, primary care follow-up, or behavioral health. This choice sets pricing, intake questions, and routing rules.
3. Smart Intake Captures Clinical Context
The platform collects symptoms, history, medications, allergies, and consent. It can also flag red-flag symptoms that require escalation.
4. Provider Availability is Matched
The system shows real-time clinicians or the next available slot. Matching can use specialty, licensure, language, and expected visit complexity.
5. One-time Payment is Completed
The patient pays per visit before the session starts. The platform confirms the transaction and generates a receipt for records or reimbursement.
6. Consultation Happens Via Video or Chat
The clinician reviews the intake, conducts the consult, and documents findings. If needed, they can switch modalities based on bandwidth or patient preference.
7. Clinical Documentation is Finalized
The platform generates a visit summary, care plan, and next steps. It also stores audit logs for clinical and compliance traceability.
8. Post-Visit Follow-Up is Triggered
The patient receives reminders, education, and escalation prompts. Enterprises can route follow-ups into care management or primary networks.
At a glance, this workflow may seem straightforward. However, its real value emerges when deployed across scale. Each step is designed to remove friction without compromising clinical safety, compliance, or financial control.
Pay-Per-Visit vs Subscription Telemedicine Models
As virtual care matures, healthcare enterprises are reassessing how telemedicine should be monetized. Subscription models gained early traction by offering predictable revenue and bundled access. However, they often struggle to match how patients actually seek care, especially for one-time or infrequent needs.
Pay-per-visit models approach the problem differently. They treat virtual care as an on-demand service, aligning cost with usage. For enterprises, the choice is less about which model is better and more about which fits specific care pathways, patient behavior, and financial objectives.
Comparison: Pay-Per-Visit vs Subscription Telemedicine
| Dimension | Pay-Per-Visit Telemedicine | Subscription Telemedicine |
| Patient Commitment | No long-term commitment | Ongoing monthly or annual plans |
| Pricing Structure | Fixed or tiered per consult | Flat recurring fees regardless of usage |
| Care Use Pattern | Episodic and urgent needs | Continuous or chronic care |
| Provider Utilization | Demand-driven and flexible | Can fluctuate with member engagement |
| Revenue Predictability | Volume-based, visit-dependent | Stable recurring revenue |
| Patient Adoption | Lower barrier to entry | Higher friction for first-time users |
| Enterprise Flexibility | Easy to layer with other models | Harder to decouple services |
| Best Fit Scenarios | Urgent care, overflow, digital front door | Chronic care, long-term programs |
Neither model is inherently superior. Each serves a different strategic purpose. Subscription-based telemedicine works well for chronic condition management and long-term patient relationships. Pay-per-visit platforms excel where speed, access, and simplicity drive adoption.
For many enterprises, the most effective approach is not choosing one over the other. It is building a platform flexible enough to support both. Pay-per-visit becomes the entry point, while subscriptions extend care continuity over time.
Business & Revenue Model of Craft
Craft’s business design reflects a clear understanding of how episodic care is consumed. Instead of pushing recurring commitments, the platform focuses on reducing friction at the moment care is needed. This approach allows Craft to scale usage while maintaining operational discipline and predictable unit economics.
Behind the interface, the model balances patient access, provider availability, and enterprise partnerships. Each layer supports growth without forcing structural changes across clinical or financial operations.
Business Models of Craft
Craft operates through multiple business configurations, depending on who consumes the service and how care is delivered.
1. Direct-to-Consumer Access
Craft offers one-time virtual visits directly to patients. Users pay only when they need care, which lowers adoption barriers and improves visit conversion rates. This model works well for urgent and first-time consultations.
2. Enterprise-Sponsored Access
Health systems and employers can sponsor visits for specific populations. Craft integrates into existing benefits or care programs without replacing primary networks. This helps enterprises extend access without increasing fixed costs.
3. Provider Network Enablement
Craft supports licensed providers by supplying demand, infrastructure, and operational tools. Clinicians focus on care delivery while the platform handles routing, payments, and documentation.
Craft’s business model succeeds because it adapts to different enterprise contexts. Whether serving individual patients or institutional partners, the platform maintains consistent workflows while allowing flexibility in how access is offered.
Revenue Models of Craft
Revenue generation on Craft is designed to scale with usage rather than subscriptions. This keeps financial performance closely tied to care delivery outcomes.
1. Per-Visit Consultation Fees
Each completed visit generates a fixed or tiered fee based on care type. Pricing varies by urgency, specialty, or service complexity, allowing revenue alignment with clinical effort.
2. Provider Revenue Sharing
Craft retains a portion of each consultation fee while paying providers per encounter. This model encourages availability during high-demand periods without inflating overhead.
3. Enterprise Contracting and Licensing
Enterprises may pay for platform access, custom workflows, or bundled visit volumes. These agreements add predictable revenue without shifting the platform away from on-demand care.
4. Value-Added Clinical Services
Additional services such as follow-up coordination, analytics, or care navigation create incremental revenue. These offerings support enterprise goals beyond single encounters.
Craft’s revenue model is built for resilience. By tying earnings to actual care usage, the platform avoids subscription fatigue while preserving financial clarity. For enterprises, this structure offers a clear line of sight between digital access, cost control, and measurable outcomes.
Telemedicine Consultation Fixed 74% Concerns In One Pay-Per-Visit
One of the most persistent concerns around pay-per-visit telemedicine is whether it truly resolves care needs or simply deflects patients temporarily.
Real-world program data suggests otherwise. Evidence from a controlled evaluation shows that on-demand telemedicine can close the majority of clinical concerns in one visit, without driving unnecessary utilization.
1. High First-Visit Resolution Rate
In a real-world evaluation involving 650 telemedicine encounters, 74% of patient concerns were resolved in a single on-demand consultation. This indicates that most episodic care needs do not require follow-up visits, referrals, or escalation.
From an enterprise perspective, this matters because first-visit resolution directly impacts cost per encounter, provider efficiency, and patient satisfaction. High closure rates reduce downstream workload and operational leakage.
2. Limited Evidence of Unnecessary Utilization
A common fear is that on-demand access creates demand that would not otherwise exist. However, only 16% of patients reported they would have done nothing if telemedicine had not been available.
This suggests the majority of visits replaced other forms of care rather than creating new demand. For pay-per-visit models, this reduces the risk of volume inflation while preserving clinical value.
3. Measurable Cost Savings Per Encounter
The same evaluation found net savings of USD 19 to USD 121 per telemedicine visit, primarily due to diversion from higher-cost settings such as urgent care centers or emergency departments.
For enterprises, these savings compound quickly at scale. Even modest adoption across episodic care pathways can translate into meaningful reductions in total cost of care.
The data shows that pay-per-visit telemedicine is not a shallow access layer. With 74% first-visit resolution, minimal evidence of unnecessary utilization, and up to USD 121 saved per encounter, the model delivers real outcomes.
Core Features of a Pay-Per-Visit Telemedicine Platform
A pay-per-visit telemedicine platform relies on tightly integrated features that enable fast access, secure care delivery, predictable payments, and enterprise-grade operational control.
For enterprises, these features collectively shape utilization, cost control, provider participation, and regulatory exposure. When designed intentionally, they transform telemedicine from a convenience tool into a dependable clinical channel.
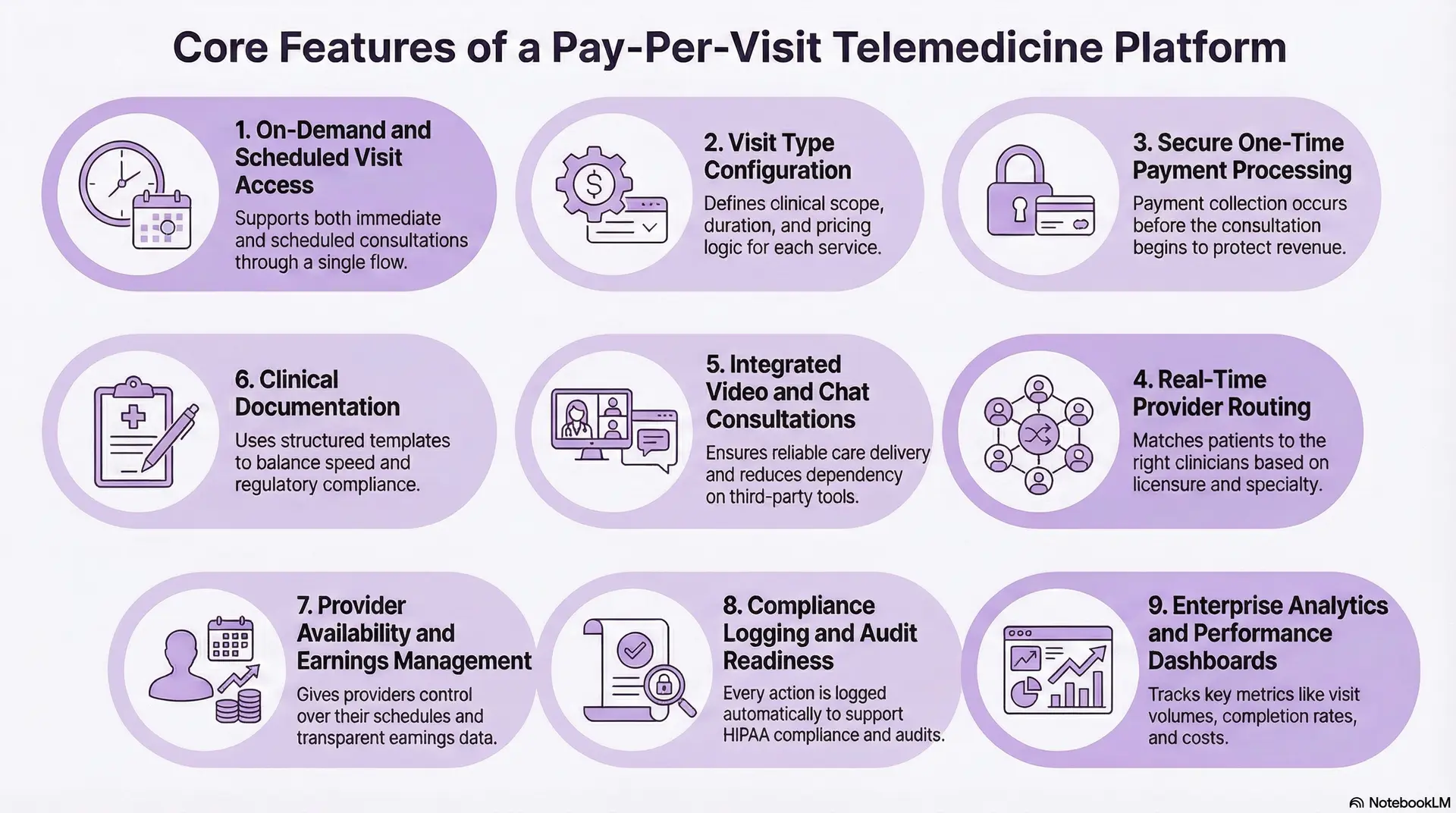
1. On-Demand and Scheduled Visit Access
A pay-per-visit platform must support both immediate and scheduled consultations through a single access flow. Patients often arrive with urgent needs, while enterprises require the ability to manage capacity and staffing over time.
This dual-access model allows organizations to serve episodic demand without overwhelming providers. It also enables after-hours coverage, overflow handling, and region-specific availability without maintaining parallel systems.
2. Visit Type Configuration
Clear visit definitions are critical in pay-per-visit care delivery. Each service line must have a predefined clinical scope, expected duration, and pricing logic.
When patients see pricing upfront, hesitation drops and visit completion increases. For enterprises, configurable pricing allows alignment between clinical effort, reimbursement expectations, and margin targets without constant operational intervention.
3. Secure One-Time Payment Processing
Payment collection must occur before the consultation begins. This protects revenue, reduces cancellations, and simplifies downstream reconciliation.
The platform should support multiple payment methods, employer-sponsored access, and payer-backed workflows where applicable. Every transaction must generate compliant receipts and audit records to support reimbursement and financial oversight.
4. Real-Time Provider Routing
Provider routing is one of the most critical operational features. The system must match patients to clinicians based on licensure, specialty, location, and case complexity.
Accurate routing reduces wait times, prevents inappropriate consults, and improves provider efficiency. Over time, this directly impacts utilization rates and patient satisfaction scores.
5. Integrated Video and Chat Consultations
Clinical interactions must remain reliable across varying network conditions and devices. Built-in video and chat reduce dependency on third-party tools and improve security posture.
The ability to transition between video and chat mid-consult ensures care continuity when connectivity issues arise. This flexibility minimizes abandoned visits and protects revenue.
6. Clinical Documentation
Documentation tools must balance speed and compliance. Providers need structured templates that reduce administrative burden while meeting regulatory standards.
After the visit, patients should receive clear summaries, prescriptions, and follow-up instructions in one secure location. This improves adherence and reduces post-visit confusion.
7. Provider Availability and Earnings Management
Providers must retain control over when and how they participate. Real-time availability management helps prevent burnout while maintaining coverage during peak periods.
Clear earnings dashboards showing completed visits, payouts, and incentives improve transparency. This visibility is essential for sustaining provider engagement in on-demand models.
8. Compliance Logging and Audit Readiness
Every action within the platform must be logged automatically. This includes access events, documentation changes, and data sharing activities.
Comprehensive audit trails support HIPAA compliance and protect enterprises during payer audits or regulatory reviews. Manual logging is not sustainable at scale.
9. Enterprise Analytics and Performance Dashboards
Leadership teams require real-time insight into how virtual care is performing. Dashboards should track visit volumes, completion rates, provider utilization, and cost per encounter.
These metrics allow enterprises to adjust staffing, pricing, and care pathways proactively. Without this visibility, telemedicine becomes reactive rather than strategic.
A pay-per-visit telemedicine platform succeeds when its features operate as a unified system. Access, payments, clinical workflows, and governance must remain aligned under real-world conditions. When built correctly, these features create a scalable digital care channel that delivers reliable access, operational control, and measurable enterprise ROI.
Data Security Requirements for Pay-Per-Visit Telemedicine Platforms
Pay-per-visit telemedicine platforms must enforce strict data security controls to protect patient information, financial transactions, and clinical records across every interaction.
For healthcare organizations, data security is not only a compliance obligation. It is a foundational requirement for operating virtual care at scale without regulatory or financial risk.
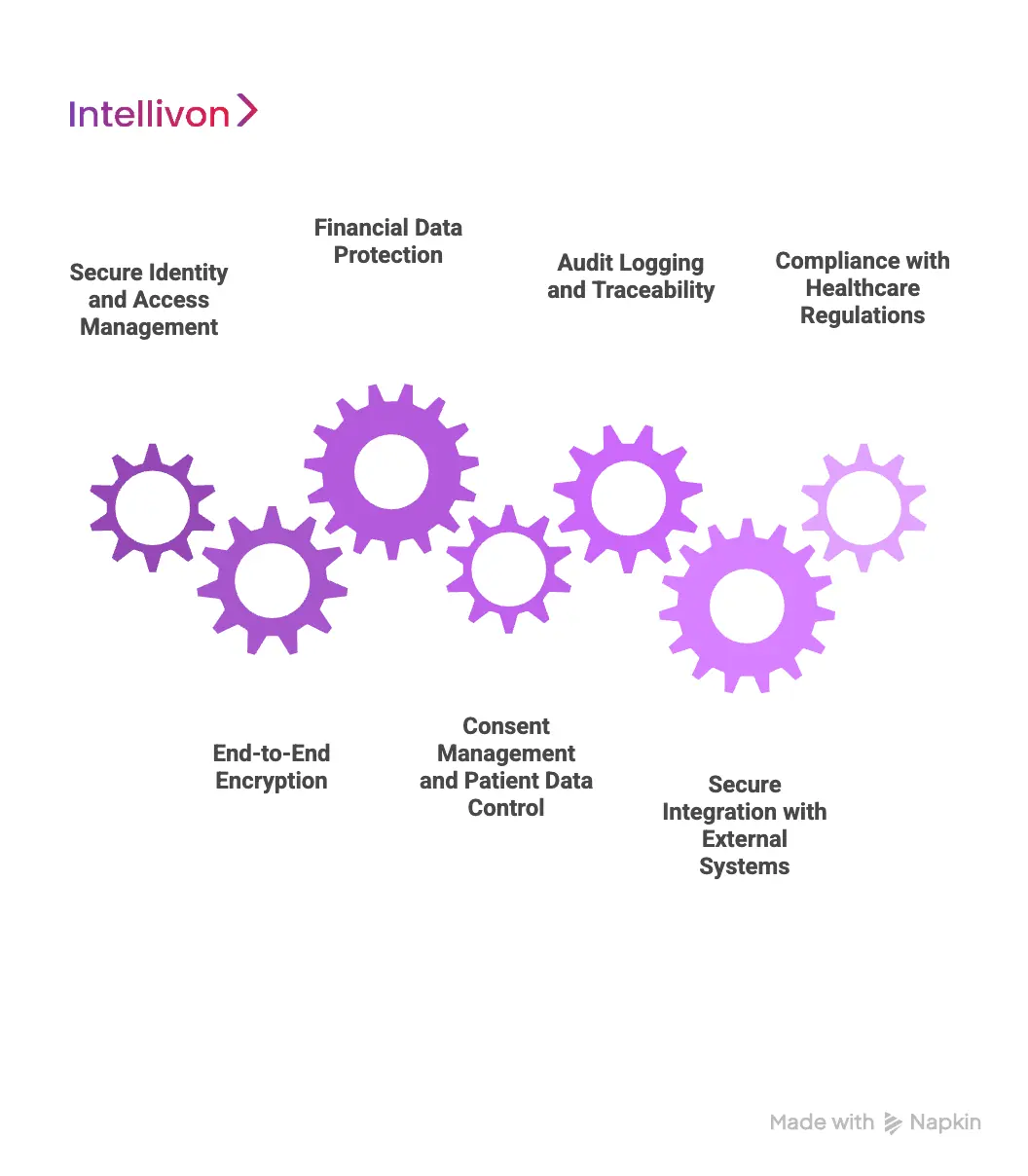
1. Secure Identity and Access Management
Every user interaction must be authenticated and authorized. Patients, providers, and administrators require different access privileges based on role and context.
Strong identity controls prevent unauthorized access to clinical data. They also ensure providers only deliver care within their licensed jurisdictions and approved scopes.
2. End-to-End Encryption
All data in transit and at rest must be encrypted using healthcare-grade standards. This includes video streams, chat messages, clinical notes, and payment details.
Encryption protects patient privacy during consultations and safeguards financial transactions. Without it, even a single breach can undermine enterprise trust.
3. Financial Data Protection
Pay-per-visit platforms handle sensitive payment information on every encounter. Payment flows must align with PCI-DSS standards and minimize exposure to card data.
Tokenization and secure payment gateways reduce risk. They also simplify audits and limit liability for healthcare organizations.
4. Consent Management and Patient Data Control
Patients must explicitly consent to data usage before care begins. The platform should capture, store, and enforce consent policies automatically.
Clear consent workflows reduce legal exposure and ensure transparency. They also support regional privacy regulations without manual intervention.
5. Audit Logging and Traceability
Every action taken within the platform must be logged. This includes access attempts, documentation changes, and data sharing events.
Comprehensive audit trails support regulatory reviews and incident investigations. They also provide accountability across clinical and administrative workflows.
6. Secure Integration with External Systems
Telemedicine platforms rarely operate in isolation. They integrate with EHRs, pharmacy systems, labs, and analytics tools.
Each integration must use secure APIs, data minimization, and strict access controls. Poorly secured integrations often become the weakest link in healthcare security.
7. Compliance with Healthcare Regulations
Pay-per-visit platforms must align with HIPAA and regional healthcare data regulations. Compliance should be embedded into system design, not added later.
Built-in safeguards reduce the risk of violations as the platform scales. They also make it easier to expand across regions and payer networks.
How AI Enhances Pay-Per-Visit Telemedicine Platforms
In a pay-per-visit telemedicine model, efficiency is not a nice-to-have. Each visit represents a single opportunity to deliver care, capture revenue, and build trust. Delays, misrouting, or incomplete documentation directly impact both patient experience and enterprise margins.
AI helps stabilize this model by removing manual friction from high-frequency workflows. When embedded across intake, routing, documentation, and analytics, AI enables platforms to scale visit volume without increasing operational overhead or clinical risk.
1. Intelligent Symptom Intake
AI-powered intake systems analyze patient-entered symptoms, demographics, and medical history before the visit begins. This transforms unstructured inputs into an organized clinical context that providers can review quickly.
By flagging potential red-flag symptoms early, AI helps ensure patients are routed to appropriate care levels. For enterprises, this reduces inappropriate virtual visits, improves visit resolution rates, and lowers downstream liability.
2. Smart Provider Matching
AI continuously evaluates provider availability, licensure, specialty, and real-time workload to route visits efficiently. It also accounts for visit complexity, expected duration, and regional demand patterns.
This reduces patient wait times while preventing provider overload. Over time, AI-driven routing creates more predictable utilization patterns, which is critical for enterprise capacity planning and cost control.
3. Real-Time Visit Assistance
During the consultation, AI can surface relevant intake details, prior visit context, and documentation prompts. This reduces cognitive switching and allows clinicians to focus on clinical decision-making rather than navigation.
The result is faster visits without rushed care. Enterprises benefit from higher visit throughput while maintaining documentation quality and consistency.
4. Automated Clinical Documentation
After the consultation, AI assists in drafting structured visit notes, care summaries, and follow-up instructions. These drafts remain clinician-reviewed to preserve clinical accountability.
This significantly shortens post-visit administrative time. It also ensures patients receive timely, consistent guidance, reducing follow-up queries and care leakage.
5. Risk Detection and Escalation Logic
AI models monitor clinical inputs and visit patterns to identify scenarios that require escalation. This may include symptoms that fall outside virtual care guidelines or repeated visits indicating unresolved issues.
Automated escalation prompts protect patient safety while ensuring virtual care is used appropriately. For enterprises, this adds a critical safety layer without manual monitoring.
6. Operational Analytics and Demand Forecasting
AI analyzes historical visit volumes, completion rates, wait times, and provider availability to predict demand trends. These insights help leaders anticipate staffing needs and adjust service coverage proactively.
Accurate forecasting reduces last-minute staffing gaps and prevents underutilization during low-demand periods. This directly impacts unit economics.
7. Fraud Detection and Abuse Prevention
AI monitors behavioral patterns across patients, providers, and payment flows to detect anomalies. This includes excessive visit frequency, unusual payment behavior, or credential misuse.
Early detection protects revenue integrity and supports compliance. It also prevents misuse that could erode trust with payers and enterprise partners.
AI strengthens pay-per-visit telemedicine platforms by making each encounter more predictable, efficient, and safe. It allows enterprises to scale on-demand care without adding operational drag or clinical exposure.
When implemented correctly, AI becomes the stabilizing layer that turns episodic virtual care into a reliable, enterprise-ready delivery model.
How We Build Pay-Per-Visit Telemedicine Platforms Like Craft
Building a pay-per-visit telemedicine platform is not a feature exercise. It is a systems problem that spans clinical safety, revenue capture, provider utilization, and regulatory accountability. Small design gaps surface quickly when every visit is transactional, and expectations are immediate.
At Intellivon, we approach platforms like Craft from an enterprise lens. Our focus is not only on launching virtual visits, but on ensuring the model holds up under real-world demand, audits, and growth. Every build decision is guided by how the platform will operate six months and three years after launch.
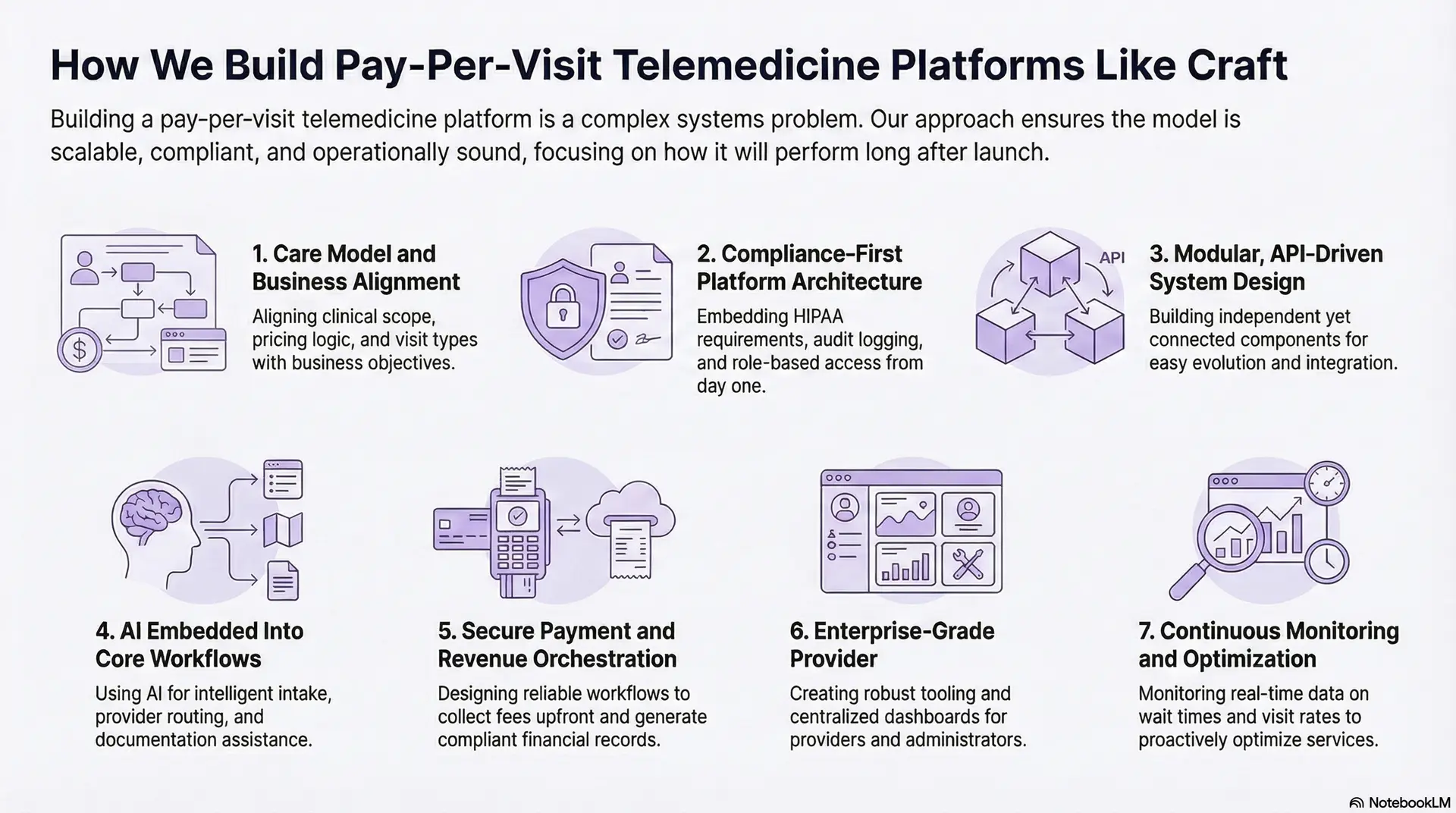
1. Care Model and Business Alignment
We begin by aligning the care model with business objectives. This includes defining visit types, clinical scope, pricing logic, and escalation rules before a single screen is designed.
By grounding the platform in real care pathways, we ensure pay-per-visit access supports urgent, episodic, and overflow care without conflicting with existing clinical programs or reimbursement strategies.
2. Compliance-First Platform Architecture
Compliance is embedded from day one. We design architecture that enforces HIPAA requirements, audit logging, role-based access, and data segregation by default.
This prevents costly retrofits later and allows enterprises to expand into new regions, payer models, or partnerships without redesigning core systems.
3. Modular, API-Driven System Design
Our platforms are built as modular services rather than monolithic applications. Scheduling, payments, video, documentation, and analytics operate as independent yet connected components.
This approach allows enterprises to evolve the platform over time. New service lines, pricing models, or employer integrations can be added without disrupting live care delivery.
4. AI Embedded Into Core Workflows
We integrate AI where it reduces friction, not where it adds complexity. This includes intelligent intake, provider routing, documentation assistance, and demand forecasting.
Each AI capability remains transparent and clinician-governed. The goal is operational efficiency with preserved clinical judgment.
5. Secure Payment and Revenue Orchestration
Pay-per-visit platforms succeed only when payments are reliable. We design payment workflows that collect fees upfront, support enterprise-sponsored access, and generate compliant financial records.
Revenue flows are tightly integrated with visit completion and provider payouts, ensuring financial clarity across stakeholders.
6. Enterprise-Grade Provider
We build tooling for providers and administrators with the same rigor as patient experiences. Providers control availability, documentation, and earnings visibility. Admin teams manage credentialing, pricing, compliance, and performance through centralized dashboards.
This operational depth allows platforms to scale without manual workarounds or fragmented oversight.
7. Continuous Monitoring and Optimization
After launch, we instrument platforms for continuous insight. Visit completion rates, wait times, provider utilization, and cost per encounter are monitored in real time.
These insights allow enterprises to optimize staffing, pricing, and care pathways proactively rather than reacting to issues after they escalate.
At Intellivon, we build pay-per-visit telemedicine platforms to operate as dependable clinical systems, not experimental products. Our approach combines compliance-first design, modular architecture, AI-enabled efficiency, and enterprise-grade governance.
For organizations looking to build platforms like Craft, success depends on more than enabling virtual visits. It requires a partner that understands how digital care, operations, and revenue intersect at scale. Intellivon brings that experience to every deployment.
Cost To Build Pay-Per-Visit Telemedicine Platforms Like Craft
Building a Craft-style pay-per-visit telemedicine platform does not require runaway budgets when approached with the right architectural and operational discipline. Cost is driven less by the number of visible features and more by how well the platform is designed around episodic care workflows, payment reliability, provider utilization, and compliance from day one.
At Intellivon, we align cost planning with enterprise budget cycles, regulatory readiness, and clear unit economics per visit. The goal is to build a pay-per-visit digital care core that can scale visit volume, service lines, and partnerships without rework or hidden operational costs.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost (USD) |
| Clinical & Business Discovery | Visit type definition, episodic care scope, provider model design, and regulatory scoping | 8,000 – 15,000 |
| Platform Architecture & Pay-Per-Visit Blueprint | System architecture, visit flow design, payment orchestration, and access control | 10,000 – 18,000 |
| Core Pay-Per-Visit Telemedicine Platform Development | Intake, visit booking, video/chat consults, one-time payment flows | 22,000 – 45,000 |
| Care Workflow & Routing Engine | Intelligent triage, provider matching, escalation and referral logic | 12,000 – 25,000 |
| Integrations & Interoperability | EHR, pharmacy, labs, identity, payment gateways | 10,000 – 20,000 |
| Security, Compliance & Governance Controls | Consent management, audit logs, role-based access, compliance validation | 8,000 – 15,000 |
| Testing, QA & Clinical Validation | Workflow testing, load testing, clinician validation | 6,000 – 10,000 |
| Pilot Deployment & Team Enablement | Controlled rollout, provider onboarding, operational tuning | 8,000 – 12,000 |
Total Initial Investment Range: USD 80,000 – 165,000
This investment supports an enterprise-grade pay-per-visit telemedicine platform deployed for one or two high-impact service lines such as urgent care or primary care access, built with strong security, compliance, and operational controls.
Annual Maintenance and Optimization Costs
Ongoing costs focus on keeping the platform secure, compliant, and efficient as visit volume grows.
- Cloud infrastructure and hosting
- Security monitoring and vulnerability patching
- Integration upkeep and API maintenance
- Workflow tuning and performance optimization
Estimated Annual Cost: 10–15% of the initial build cost
Approximately USD 8,000 – 25,000 per year
Platforms that invest early in interoperability and compliance engineering experience the most predictable operating costs.
Cost Variables to Plan for During Scale
As adoption increases, additional cost drivers may emerge, including:
- Expanding visit types or clinical specialties
- Adding behavioral health or specialty consults
- Higher video usage and data storage volumes
- Multi-state or multi-region regulatory coverage
- Advanced analytics and AI-assisted optimization
Anticipating these variables early prevents budget pressure during growth phases.
How Enterprises Stay Within the USD 80K–165K Range
Healthcare organizations that manage pay-per-visit telemedicine costs effectively tend to:
- Launch with a focused set of visit types and clear clinical boundaries
- Limit regional complexity in the initial phase
- Design pricing and payment logic upfront
- Use modular architecture to expand incrementally
- Track cost per encounter and provider utilization within the first 60–90 days
This approach ensures the platform demonstrates both operational and financial value before larger capital deployment.
Talk to Intellivon’s healthcare platform architects to receive a phased cost estimate aligned with your enterprise growth strategy and pay-per-visit care roadmap.
Common Challenges in Building Pay-Per-Visit Telemedicine Platforms
Enterprises building pay-per-visit telemedicine platforms face operational, clinical, and financial challenges that require compliance-first design and disciplined execution.
Addressing these challenges requires more than feature development. It demands deep alignment between clinical workflows, payment logic, provider operations, and compliance. Below are the most common enterprise-level challenges and how Intellivon helps resolve them.
1. Inconsistent Provider Availability
One of the most common challenges is maintaining consistent provider availability during fluctuating demand. In pay-per-visit models, patient expectations are immediate, yet provider supply often varies by time, region, and specialty.
At Intellivon, we design availability controls, intelligent routing, and utilization analytics that help enterprises balance demand without overstaffing. This ensures access remains reliable while protecting provider experience and cost efficiency.
2. Revenue Leakage and Payment Failures
Upfront payment is critical in pay-per-visit care, but poorly designed flows can lead to failed transactions, abandoned visits, and reconciliation gaps. These issues directly impact margins and trust.
Intellivon builds secure, pre-visit payment orchestration with clear failure handling and audit trails. This approach reduces no-shows, improves revenue capture, and simplifies financial oversight.
3. Clinical Risk and Inappropriate Virtual Care
Not all conditions are suitable for virtual treatment. Without strong triage and escalation logic, platforms risk misdirected care and increased liability.
We embed clinical guardrails, AI-assisted triage, and escalation pathways into the core workflow. This ensures patients receive appropriate care while protecting enterprises from regulatory and clinical exposure.
4. Scaling Without Operational Chaos
As visit volume grows, manual workflows break down. Credentialing, compliance checks, and reporting often become bottlenecks that slow expansion.
Intellivon designs platforms with automated governance, modular services, and real-time analytics. This enables enterprises to scale visit volume and service lines without operational sprawl.
5. Regulatory and Compliance Complexity
Telemedicine regulations vary by region, payer, and care type. Managing licensure, consent, and audit readiness across jurisdictions is a persistent challenge.
Our compliance-first architecture embeds regulatory controls directly into system design. This reduces risk, simplifies audits, and supports expansion across markets.
6. Fragmented Data and Limited Visibility
Without unified data, leadership teams struggle to assess performance, cost per visit, and care outcomes. Fragmentation limits strategic decision-making.
Intellivon delivers centralized dashboards and integrated data pipelines that provide real-time insight into clinical, operational, and financial metrics. This visibility enables proactive management rather than reactive fixes.
Building a pay-per-visit telemedicine platform requires navigating challenges that cut across care delivery, finance, and compliance. Enterprises that succeed treat these challenges as design constraints, not afterthoughts.
Conclusion
Pay-per-visit telemedicine has moved beyond convenience. It has become a strategic care delivery model for enterprises that need flexible access, controlled costs, and reliable operations. When designed correctly, it aligns patient behavior with provider availability and measurable unit economics.
Success depends on more than launching virtual visits. It requires disciplined architecture, embedded compliance, and workflows built for real-world demand. Platforms like Craft demonstrate what is possible when these elements come together.
For organizations ready to scale episodic virtual care, execution matters as much as intent. With the right partner, pay-per-visit telemedicine becomes a growth enabler rather than an operational risk.
Build Your Pay-Per-Visit Telemedicine Platform With Intellivon
At Intellivon, we build pay-per-visit telemedicine platforms as enterprise operating systems, not isolated virtual visit tools layered onto legacy workflows. Our platforms are designed to function as a governed digital access layer, connecting on-demand care, secure payments, provider operations, and downstream clinical services into one controlled system.
Each solution is engineered for healthcare enterprises that require flexibility without loss of control. Platforms are infrastructure-first, compliance-led, and built to handle fluctuating visit demand while delivering predictable unit economics, protected provider capacity, and measurable ROI as virtual care scales across service lines and regions.
Why Partner With Intellivon?
- Pay-per-visit care architecture aligned with episodic workflows, pricing governance, and provider utilization control
- Deep interoperability expertise across EHRs, identity systems, HL7, FHIR, pharmacy, labs, and payment ecosystems
- Compliance-by-design platforms supporting HIPAA, consent lifecycle management, licensure controls, and audit-ready operations
- AI-enabled care orchestration for intake intelligence, visit routing, documentation support, and demand forecasting
- Enterprise-scale delivery model with phased rollout, cost predictability, and continuous performance optimization
Talk to Intellivon’s healthcare platform architects to explore how a Craft-style pay-per-visit telemedicine platform can expand access, control costs, and scale episodic digital care with confidence.
FAQs
Q1. What is a pay-per-visit telemedicine platform?
A1. A pay-per-visit telemedicine platform allows patients to access virtual care on demand and pay once per completed consultation. Unlike subscription models, it supports episodic care, urgent access, and overflow demand without long-term commitments.
Q2. How is a pay-per-visit telemedicine model different from subscription telehealth?
A2. Pay-per-visit telemedicine charges per encounter and aligns cost with usage. Subscription telehealth relies on recurring fees and works better for continuous or chronic care programs rather than one-time clinical needs.
Q3. How much does it cost to build a pay-per-visit telemedicine platform?
A3. Enterprise-grade pay-per-visit telemedicine platforms typically cost between USD 80,000 and 165,000 to build. Final cost depends on care scope, compliance requirements, integrations, and AI capabilities.
Q4. What regulations apply to pay-per-visit telemedicine platforms?
A4. These platforms must comply with HIPAA, regional telemedicine laws, provider licensure rules, consent management requirements, and payment security standards such as PCI-DSS for financial transactions.
Q5. Is pay-per-visit telemedicine suitable for large healthcare enterprises?
A5. Yes. Pay-per-visit models work well for urgent care, episodic access, after-hours coverage, and digital front-door strategies. When built correctly, they integrate with enterprise systems and scale without operational disruption.