Hospital networks still depend on disconnected platforms pieced together over time. Patient data can flow, but governance often does not keep pace. A discharge may be completed in the clinical system, but revenue capture can lag behind. Inventory updates in pharmacy happen, but procurement forecasts remain outdated.
As hospital groups grow across regions and reimbursement models shift toward value-based care, these disconnects lead to more than just inefficient workflows. They reveal financial losses, compliance gaps, operational blind spots, and audit risks.
A strong hospital management system must do more than manage departments. It should coordinate clinical operations, revenue governance, interoperability standards, and security controls as a single infrastructure layer. It needs to link real-time hospital events to billing logic, compliance enforcement, audit trails, and analytics without causing reintegration issues.
At Intellivon, we create hospital management systems as an enterprise healthcare infrastructure, not just departmental software. We prioritize architecture, governance is built in, and interoperability is carefully designed from the ground up. In this guide, we will explain what truly makes a hospital management system enterprise-ready, how compliance and middleware influence its design, and what it takes to create a scalable, secure platform.
Why Enterprises Are Investing in Hospital Management Systems Now
Healthcare enterprises are increasing investment in hospital management systems to control rising operating costs, address clinician shortages, and meet growing demands for data-driven care under value-based reimbursement models.
These integrated platforms connect patient management, revenue cycle operations, and inventory control into a unified system, which reduces manual effort and improves coordination across departments. As a result, many organizations report efficiency gains of 20 to 30% while strengthening financial oversight and operational visibility.
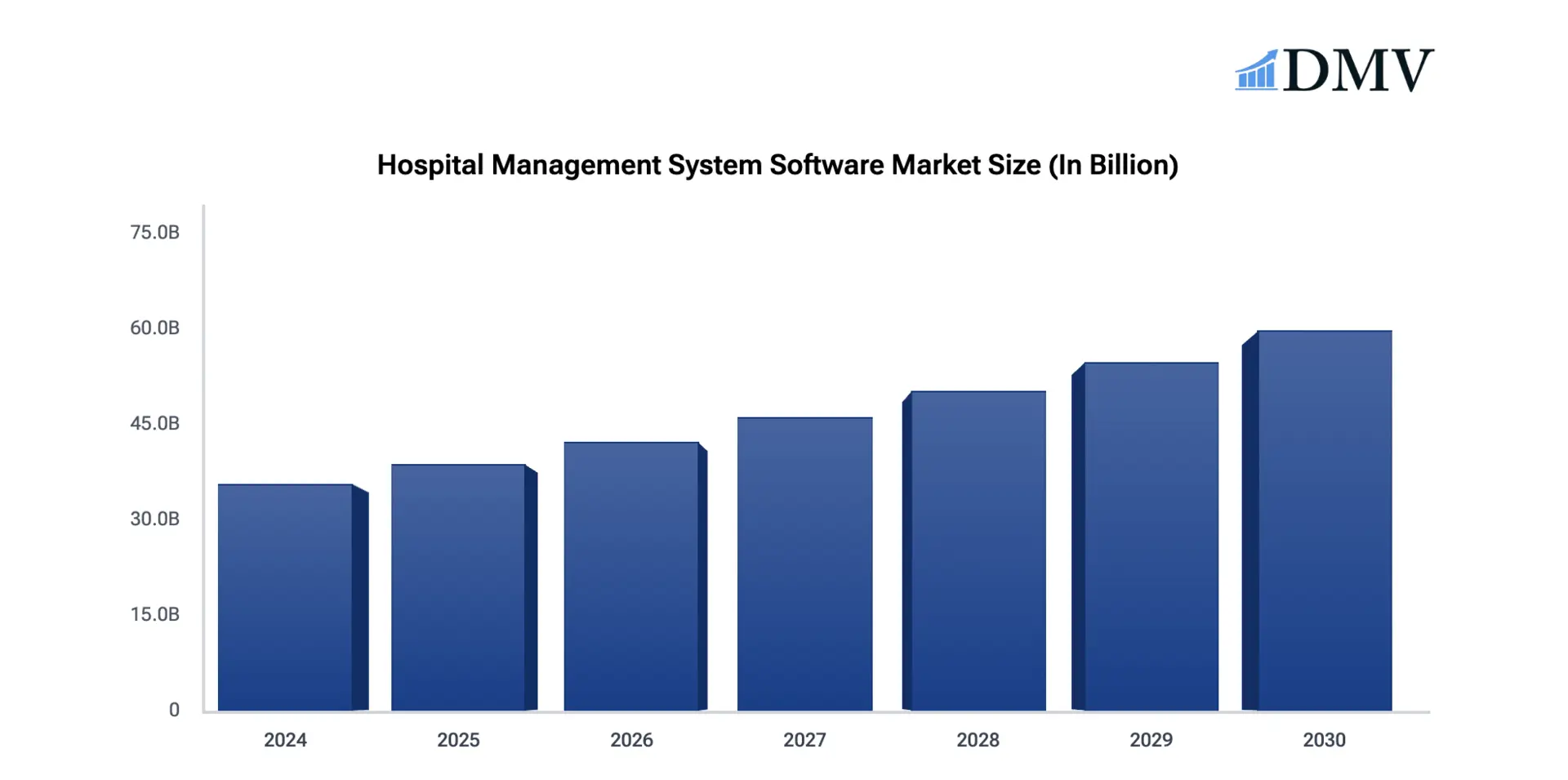
The global hospital management system software market continues to expand rapidly and is projected to reach $35.6 billion in 2024. Analysts estimate a compound annual growth rate of 9.2 %, reflecting sustained demand and steady modernization across healthcare enterprises.
Market Insights:
- Automation across scheduling, billing, and administrative workflows can reduce processing errors by more than 50%.
- AI and machine learning capabilities now support predictive patient flow management, smarter capacity planning, and clinical decision support. In addition, interoperability with EHR systems strengthens TEFCA alignment and enables real-time analytics across departments.
- With medical errors contributing to more than 250,000 deaths annually in the United States, and aging populations increasing care demand, healthcare organizations require scalable digital infrastructure that improves oversight while controlling costs.
More than 80% of large hospitals now rely on cloud-based hospital management systems, a shift accelerated by remote access needs and rapid digitization during COVID. Consequently, distributed teams can manage clinical and operational workflows securely across multiple locations without infrastructure constraints.
At the same time, over 70% of healthcare enterprises show strong interest in AI-driven decision support, while patient management modules grow at more than 13% annually. Although upfront investment remains a concern, documented time savings of 20 to 40% across administrative functions continue to justify enterprise adoption.
What Is an Enterprise-Grade Hospital Management System?
An enterprise-grade hospital management system is a centralized digital platform that manages clinical operations, revenue cycles, supply chains, compliance controls, and reporting across one or multiple hospital entities. It connects departments such as admissions, pharmacy, diagnostics, billing, and administration into a single governed environment.
Unlike basic hospital software, it supports interoperability with EHRs, insurers, laboratories, and government systems through secure APIs and data standards. It also embeds audit trails, access controls, and regulatory safeguards from the start.
As hospitals expand, this system scales with them. Therefore, it becomes core operational infrastructure, not just administrative software.
Enterprise HMS vs Traditional Hospital Software
Enterprise healthcare organizations often outgrow traditional hospital software faster than expected. What works for a single facility rarely supports a multi-location network with shared governance, centralized reporting, and cross-site coordination. Therefore, leaders must evaluate whether their current system can scale with strategic expansion.
Traditional platforms usually focus on departmental efficiency. In contrast, enterprise hospital management systems align operations, finance, compliance, and analytics under one governed framework. As complexity increases, this distinction becomes critical.
| Criteria | Traditional Hospital Software | Enterprise HMS |
| Architecture | Monolithic, single-site setup | Modular, scalable, multi-entity architecture |
| Integration | Limited EHR and API support | Interoperable with EHRs, payers, HIEs, and external systems |
| Compliance | Basic reporting tools | Built-in audit trails, access control, policy enforcement |
| Scalability | Designed for one hospital | Designed for networks, mergers, and regional growth |
| Analytics | Static reports | Real-time dashboards and predictive insights |
| Governance | Department-driven | Enterprise-wide visibility and control |
As hospitals expand across regions, governance gaps widen if systems remain siloed. Consequently, enterprise-grade infrastructure becomes a strategic necessity rather than a technology upgrade. The choice determines whether growth creates coordination or chaos.
What Enterprise Problems A Hospital Management System Solves
An enterprise hospital management system solves fragmented workflows, revenue leakage, compliance gaps, and poor operational visibility across multi-hospital networks.
As hospital networks expand, operational complexity grows quickly. Departments operate on different systems. Data lives in silos. Leadership lacks real-time visibility. As a result, delays, errors, and financial leakage become common. An enterprise hospital management system addresses these structural problems at scale.
1. Fragmented Workflows Across Departments
Many hospitals still rely on disconnected systems for admissions, pharmacy, billing, and diagnostics.
Therefore, information does not move smoothly between teams. An integrated platform connects these workflows in real time. Consequently, staff reduce duplication and avoid costly handoff errors.
2. Revenue Cycle Leakage and Billing Delays
Missed charges, coding errors, and delayed claims impact margins. In addition, value-based reimbursement increases financial pressure.
A unified system automates billing logic and links it directly to clinical events. As a result, organizations improve claim accuracy and accelerate cash flow.
3. Lack of Real-Time Operational Visibility
Enterprise leaders need visibility across bed capacity, inventory, and patient flow. However, static reports often arrive too late.
A modern HMS provides live dashboards and centralized reporting. Therefore, decisions are based on current data, not outdated summaries.
4. Compliance and Audit Risk
Healthcare regulations demand traceability and strict access control. When systems are fragmented, audit readiness becomes difficult.
An enterprise-grade platform embeds role-based access, policy enforcement, and detailed logs. Consequently, organizations strengthen compliance without adding manual oversight.
5. Scalability Challenges During Growth
Mergers, expansions, and new service lines increase operational load. Traditional systems struggle to adapt.
In contrast, a scalable hospital management system supports multi-site governance and standardized processes. Therefore, growth becomes controlled and sustainable.
In short, an enterprise hospital management system reduces operational friction while strengthening financial and regulatory control. For expanding healthcare organizations, it becomes foundational infrastructure rather than optional software.
Essential Features of an Enterprise Hospital Management System
Enterprise hospital management systems combine scalable architecture, interoperability, revenue automation, real-time analytics, and embedded compliance controls to support multi-hospital governance.
Enterprise healthcare organizations operate across multiple departments, facilities, and regulatory environments. Therefore, their hospital management systems must support scale, control, and coordination from the foundation.
Below are the core features that distinguish enterprise-grade platforms from basic operational tools.
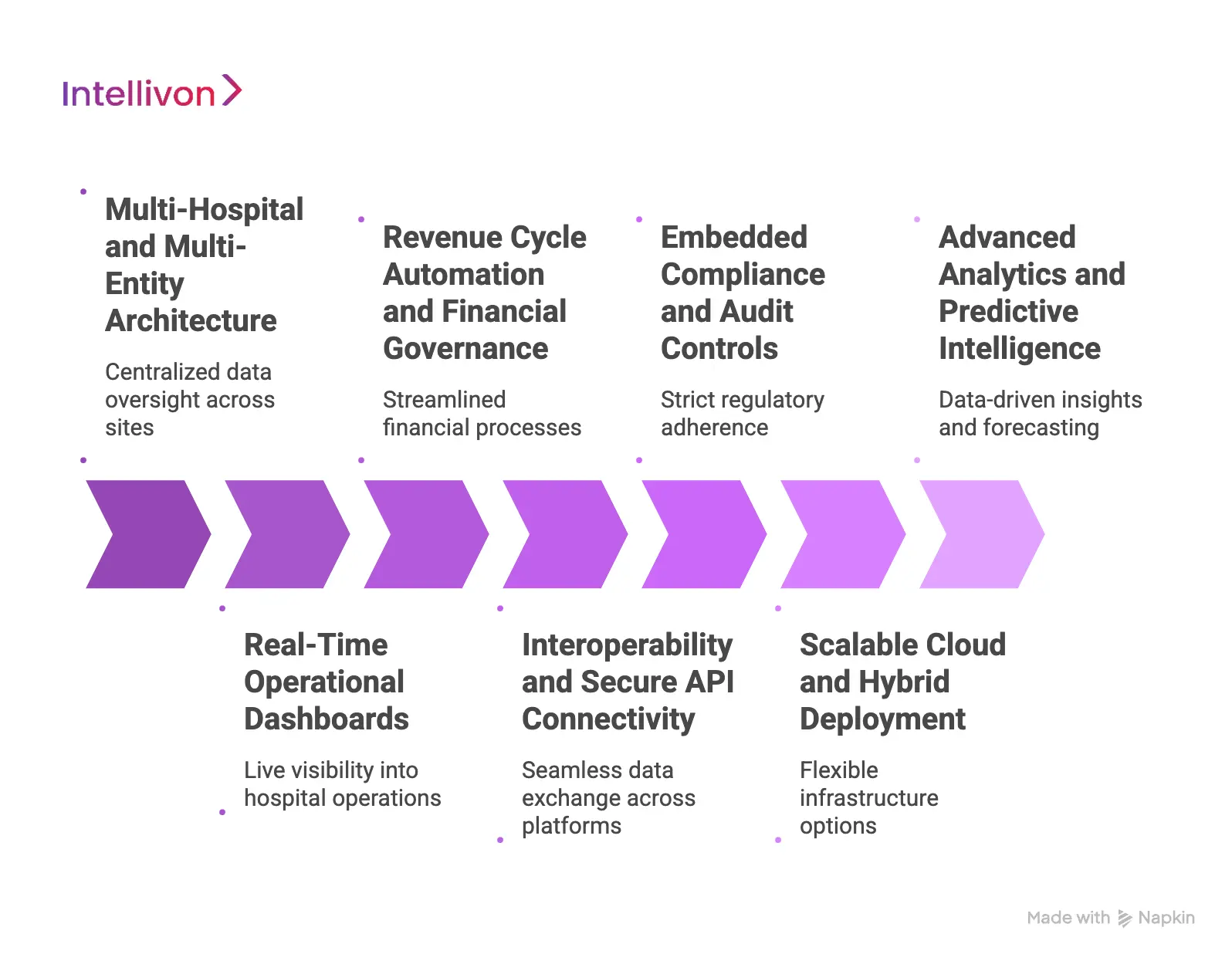
1. Multi-Hospital and Multi-Entity Architecture
An enterprise system must support several hospitals, clinics, and specialty units under a single governance model. This structure allows centralized data oversight while preserving local operational workflows.
In addition, leadership can standardize policies, reporting formats, and performance metrics across sites. When mergers or expansions occur, new entities can be added without rebuilding the system. As a result, growth becomes structured rather than disruptive.
2. Real-Time Operational Dashboards
Enterprise leaders require live visibility into patient flow, bed capacity, emergency department load, operating room utilization, and staffing patterns. Static monthly reports do not support fast decisions.
Therefore, modern systems provide real-time dashboards with drill-down capability. Alerts notify teams when thresholds are crossed, such as occupancy limits or inventory shortages. Consequently, decision-making shifts from reactive to proactive.
3. Revenue Cycle Automation and Financial Governance
Revenue integrity is critical under value-based reimbursement models. Enterprise-grade systems connect clinical documentation, coding logic, billing workflows, and claims submission in one unified process.
In addition, automated validation checks reduce human error before claims are sent to payers. Finance teams gain visibility into outstanding claims, denial rates, and reimbursement cycles. Therefore, margins improve while compliance risks decrease.
4. Interoperability and Secure API Connectivity
Hospitals operate within a broader digital ecosystem that includes EHR platforms, laboratories, pharmacies, insurers, and government systems. An enterprise hospital management system must support HL7, FHIR, and secure API integrations.
This ensures structured data exchange across internal and external platforms. In addition, standardized interoperability reduces manual reconciliation work. As a result, patient information flows consistently across the care continuum.
5. Embedded Compliance and Audit Controls
Healthcare regulations require strict access control, audit logging, and data protection measures. Enterprise platforms integrate role-based access management, encryption, and automated policy enforcement from the start. Every system action is traceable, which simplifies audits and investigations.
Moreover, centralized governance ensures consistent compliance across facilities. Therefore, regulatory readiness becomes part of daily operations rather than a separate exercise.
6. Scalable Cloud and Hybrid Deployment
Enterprise hospitals often operate across regions with varying infrastructure needs. A modern system supports cloud, hybrid, or on-premise deployment models. This flexibility allows secure remote access while maintaining local control where required.
In addition, disaster recovery and high-availability architecture protect operations during outages. Consequently, uptime and business continuity remain stable even during high patient volumes.
7. Advanced Analytics and Predictive Intelligence
Operational data alone is not enough; enterprises need insights. Enterprise-grade platforms include analytics engines that forecast patient demand, identify resource gaps, and highlight financial risks.
AI-driven models can predict admission trends and optimize staffing. Therefore, leaders make informed decisions based on patterns rather than assumptions. Over time, data becomes a strategic asset rather than just a record-keeping tool.
Together, these features transform a hospital management system from a departmental tool into an enterprise infrastructure. When aligned correctly, they support operational efficiency, financial control, and scalable growth across complex healthcare networks.
Compliance and Security Frameworks in Enterprise HMS
Enterprise hospital management systems must embed compliance, cybersecurity, audit controls, and data governance into their architecture to protect patient data and reduce regulatory risk.
Regulation shapes every healthcare operation. Therefore, an enterprise hospital management system must treat compliance and security as structural requirements, not afterthoughts. When systems scale across facilities and regions, risk multiplies quickly. A weak access policy or a missing audit trail can expose the entire network.
Below are the core frameworks and controls that define enterprise readiness.
1. Regulatory Alignment and Policy Enforcement
Healthcare organizations operate under strict data protection and reporting laws. These include HIPAA, HITECH, regional health data regulations, and payer mandates. An enterprise HMS must map workflows to these regulatory requirements from day one.
In addition, policy enforcement should be automated. For example, access restrictions and documentation checks should trigger system controls, not manual reminders. Consequently, compliance becomes part of routine operations rather than a separate administrative burden.
2. Role-Based Access and Identity Governance
Large hospital networks involve thousands of users. Doctors, nurses, finance teams, and administrators require different system permissions. Therefore, role-based access control is essential.
An enterprise system assigns privileges based on job function and location. Moreover, identity governance tracks user activity across departments. If a breach occurs, leadership can quickly trace access history and respond effectively.
3. Data Encryption and Zero-Trust Security
Patient records contain highly sensitive information. Enterprise platforms must encrypt data both at rest and in transit. However, encryption alone is not sufficient.
Modern security architecture follows a zero-trust model. Every access request is verified, even within internal networks. As a result, unauthorized movement inside the system becomes far more difficult.
4. Audit Trails and Traceability
Regulators and payers demand clear documentation. Therefore, every action inside the hospital management system must be logged. This includes data edits, billing updates, and access attempts.
Comprehensive audit trails allow leadership to reconstruct events quickly. In addition, automated reporting tools simplify compliance reviews. Consequently, audit preparation no longer disrupts daily operations.
5. Disaster Recovery and Business Continuity
Enterprise healthcare operations cannot afford downtime. Power outages, cyber incidents, or infrastructure failures can halt care delivery. Therefore, enterprise HMS platforms must include redundancy, failover systems, and real-time data backup.
High-availability architecture ensures continuity even during regional disruptions. Moreover, tested recovery protocols reduce operational shock when incidents occur.
6. Data Governance Across Multi-Site Networks
As hospital groups expand, consistent governance becomes challenging. An enterprise system centralizes data standards, retention policies, and reporting structures across all facilities.
This consistency reduces reporting discrepancies and strengthens enterprise oversight. Over time, governance shifts from reactive problem-solving to structured control.
In enterprise healthcare, compliance and security define operational credibility. When embedded correctly, they protect not only patient data but also financial stability and brand reputation.
Integration with EHR and External Healthcare Ecosystems
An enterprise hospital management system must integrate seamlessly with EHRs, payers, labs, and digital health platforms to ensure secure, real-time data exchange across the care ecosystem.
Hospitals do not operate in isolation. Clinical care, billing, insurance processing, laboratory services, and government reporting all rely on connected systems. Therefore, an enterprise hospital management system must integrate smoothly with EHR platforms and external partners. Without this connectivity, data gaps slow care delivery and create financial risk.
1. Seamless EHR Connectivity
Electronic health records sit at the center of clinical documentation. An enterprise HMS must exchange structured data with EHR platforms using standards such as HL7 and FHIR. This ensures patient admissions, lab orders, discharge summaries, and billing events stay synchronized.
In addition, real-time integration reduces manual reconciliation between systems. As a result, clinical and administrative teams work from the same source of truth.
2. Payer and Insurance System Integration
Revenue cycle performance depends on accurate and timely claims submission. Therefore, integration with insurer portals and clearinghouses is critical.
A connected system links clinical documentation to coding and claims workflows automatically. Consequently, hospitals reduce denial rates and improve reimbursement timelines. Finance teams gain visibility without switching between multiple platforms.
3. Laboratory, Pharmacy, and Diagnostic Interfaces
Hospitals rely on external labs and imaging centers for diagnostic services. An enterprise HMS must support secure interfaces that transmit orders and receive results in real time.
This integration improves turnaround time and reduces errors caused by manual data entry. In addition, inventory systems can align automatically with pharmacy and supply chain updates.
4. Health Information Exchange and Regional Networks
Many healthcare systems participate in regional or national health information exchanges. Therefore, the hospital management platform must support standardized data sharing.
This enables cross-hospital collaboration, referral tracking, and coordinated patient care. As networks grow, interoperability ensures continuity rather than fragmentation.
5. Digital Health and Remote Care Platforms
Telemedicine apps, remote monitoring tools, and patient engagement portals continue to expand. An enterprise HMS should connect with these platforms through secure APIs.
Consequently, patient data flows consistently across virtual and in-person care environments. Leadership gains unified visibility into the entire care journey.
Strong integration transforms a hospital management system into a connected enterprise platform. When systems communicate securely and in real time, operational efficiency improves, and patient outcomes follow.
How We Develop Enterprise-Grade Hospital Management Systems
Enterprise hospital systems demand structured execution. At Intellivon, we approach development as infrastructure engineering. Each step is designed to reduce operational risk while enabling long-term scalability and control. Below is the seven-step framework we follow.
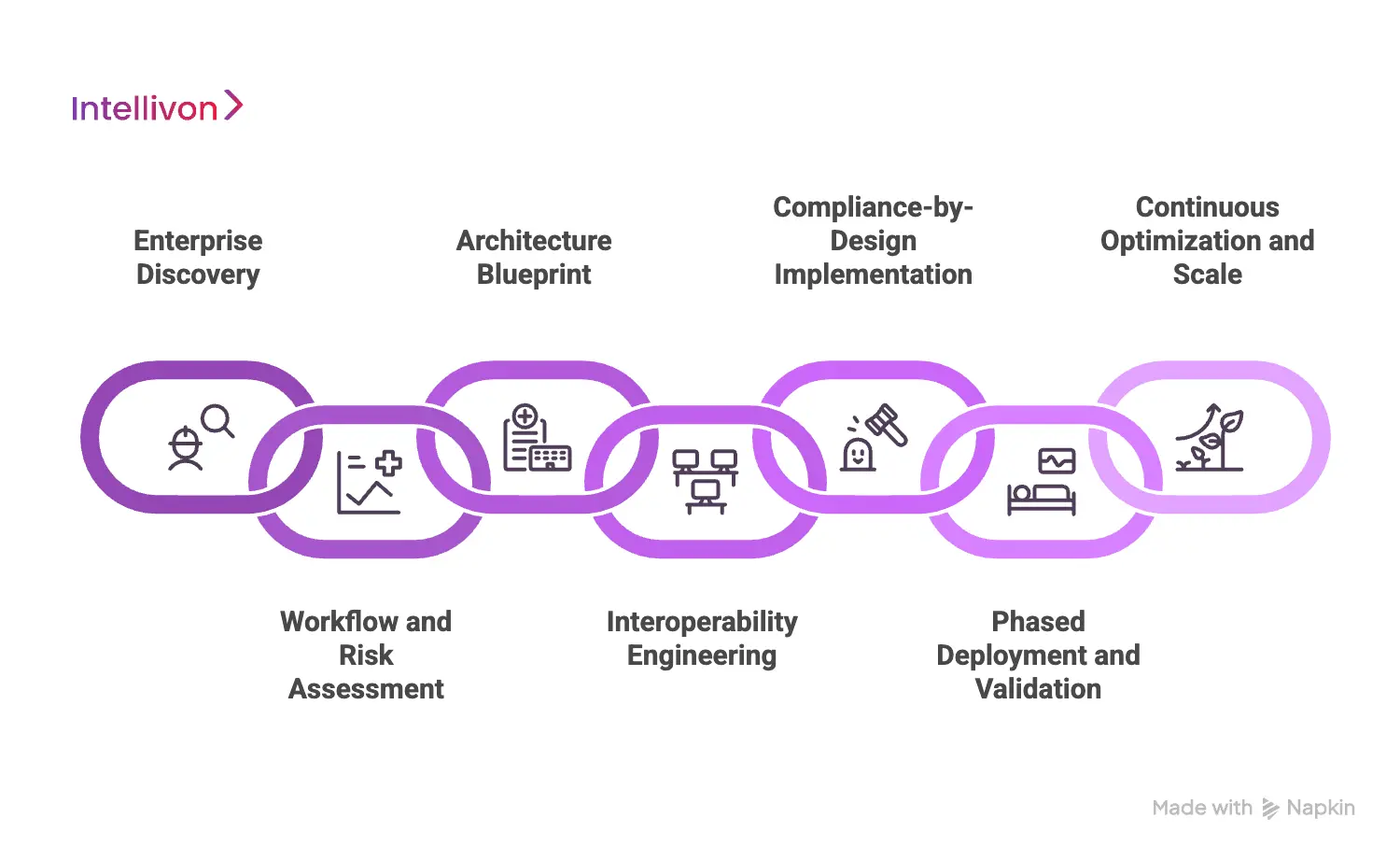
1. Enterprise Discovery
We begin by understanding your operating model, expansion plans, and regulatory obligations. This includes stakeholder interviews, workflow mapping, and system audits.
In addition, we review financial reporting structures and integration dependencies. Therefore, every design decision aligns with the enterprise strategy rather than isolated requirements.
2. Workflow and Risk Assessment
Next, we assess clinical, administrative, and revenue workflows in detail. We identify breakdown points, manual handoffs, and compliance gaps.
Moreover, we evaluate data accuracy and reporting inconsistencies. As a result, leadership gains a clear view of where inefficiencies create financial and operational strain.
3. Architecture Blueprint
We then design a scalable, modular architecture that supports multi-hospital governance. This includes defining microservices layers, data models, access controls, and infrastructure strategy.
Security frameworks are embedded from the start. Consequently, the system can expand without structural redesign.
4. Interoperability Engineering
Integration is structured using standardized protocols such as HL7 and FHIR. We design secure API layers that connect EHRs, payers, labs, and digital platforms.
In addition, middleware orchestration ensures controlled data exchange between departments. Therefore, interoperability remains stable even as external systems evolve.
5. Compliance-by-Design Implementation
Regulatory controls are woven into system workflows, not layered afterward. Role-based access, audit logging, encryption, and policy enforcement operate automatically.
This approach reduces manual oversight and strengthens regulatory readiness. As a result, compliance becomes operational rather than reactive.
6. Phased Deployment and Validation
Enterprise rollouts are executed in controlled phases. Critical workflows run in parallel during the transition to prevent service disruption.
Performance, security, and integration points are continuously monitored. Consequently, teams gain confidence while minimizing downtime risk.
7. Continuous Optimization and Scale
After go-live, we track operational metrics, system performance, and user adoption. Data insights guide refinements and feature enhancements.
As hospital networks expand, new facilities and service lines integrate into the existing framework seamlessly. Therefore, the platform evolves alongside the enterprise.
Through this structured seven-step framework, Intellivon delivers hospital management systems that scale securely while maintaining financial, clinical, and regulatory control.
The result is a durable enterprise infrastructure that supports growth, reduces risk, and strengthens operational performance over time.
Cost Of Building An Enterprise-Grade Hospital Management Systems
At Intellivon, enterprise hospital management systems are engineered as regulated healthcare infrastructure, not as departmental software layered onto legacy tools. The focus remains on unifying clinical workflows, revenue governance, interoperability, analytics, and compliance controls within one scalable environment.
When budget constraints exist, scope is prioritized carefully. However, security architecture, audit frameworks, access governance, and interoperability layers are never compromised.
Therefore, organizations avoid reintegration expenses and regulatory exposure that surface after fragmented implementations. Predictability replaces reactive spending, and long-term ROI remains protected.
Estimated Phase-Wise Investment Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Enterprise Discovery & Workflow Mapping | Operational assessment, financial process review, integration mapping, compliance evaluation | $8,000 – $15,000 |
| Architecture & Infrastructure Blueprint | Multi-site design, deployment model selection, scalability modeling | $10,000 – $18,000 |
| Interoperability Engineering | HL7/FHIR integration, API framework, data normalization | $8,000 – $15,000 |
| Revenue & Clinical Module Development | Admissions, billing, pharmacy, inventory, reporting engines | $10,000 – $22,000 |
| Governance & Compliance Framework | Role-based access, audit trails, encryption, policy controls | $6,000 – $12,000 |
| Security Hardening & Testing | Penetration testing, validation, and performance optimization | $4,000 – $8,000 |
| Deployment & Scale Enablement | Cloud or hybrid rollout, system tuning, and user onboarding | $4,000 – $10,000 |
Total initial investment: $50,000 – $150,000
Ongoing maintenance and optimization: Approximately 15–20% of the initial build annually
Hidden Cost Drivers Enterprises Should Anticipate
Even structured programs can experience financial pressure when indirect drivers are overlooked. Early planning reduces budget drift.
- Integration complexity increases as hospital networks expand
- Compliance monitoring intensifies with regulatory updates
- Data migration from legacy systems requires validation cycles
- Infrastructure usage grows with transaction and patient volume
- Change management demands structured training and adoption programs
- Continuous monitoring and analytics scale with operational growth
Best Practices to Control Investment and Risk
Based on Intellivon’s enterprise delivery experience, the following principles protect long-term value:
- Standardize workflows before digitizing them
- Architect interoperability early to prevent costly retrofits
- Embed compliance controls within core system logic
- Use modular components that support phased expansion
- Maintain observability across financial and clinical indicators
- Plan for regulatory evolution, not static certification
Request a tailored proposal from Intellivon’s enterprise healthcare specialists to receive a roadmap aligned with your strategic priorities, compliance obligations, and digital transformation goals.
How Enterprise Hospital Management Systems Will Evolve in the Future
Hospital management systems are moving beyond administrative coordination. As healthcare networks expand and reimbursement models evolve, these platforms must shift from record management to intelligent orchestration. Therefore, future systems will focus on automation, predictive insight, and enterprise-wide governance.
Below are the key directions shaping the next generation of enterprise platforms.
1. AI-Driven Operational Orchestration
AI will increasingly manage patient flow, staffing alignment, and resource allocation. Instead of reacting to congestion, systems will forecast demand patterns in advance.
In addition, machine learning models will identify revenue risks and compliance anomalies early. As a result, leadership will move from reactive decision-making to proactive optimization.
2. Predictive Capacity and Demand Planning
Future platforms will analyze historical trends, demographic shifts, and seasonal patterns. This will support accurate forecasting for bed capacity, operating room schedules, and emergency department loads.
Consequently, hospitals can plan staffing and inventory with greater precision. Cost control will improve without compromising patient access.
3. Deeper Interoperability Across Ecosystems
Interoperability will expand beyond EHR connectivity. Enterprise systems will integrate seamlessly with regional health networks, remote monitoring tools, digital therapeutics, and payer analytics engines.
Therefore, patient data will move securely across the entire care continuum. This connectivity will strengthen coordinated care and value-based reporting.
4. Embedded Governance Automation
Compliance requirements will continue to grow. Future systems will automate policy enforcement, documentation validation, and audit readiness in real time. Instead of periodic reviews, governance controls will operate continuously.
Consequently, regulatory oversight becomes operationally embedded rather than administratively managed.
5. Intelligent Financial Optimization
Revenue cycle modules will incorporate predictive denial management and automated reimbursement analytics. Systems will flag coding inconsistencies before submission.
In addition, financial dashboards will link clinical decisions directly to margin impact. Therefore, enterprises will gain clearer visibility into profitability drivers.
6. Scalable Cloud and Distributed Infrastructure
Cloud-native design will dominate enterprise deployments. However, hybrid models will remain relevant for regional compliance needs.
Systems will support distributed access with centralized control. As healthcare networks expand across regions, infrastructure flexibility will become essential.
The future of enterprise hospital management systems lies in structured intelligence and continuous coordination. Organizations that adopt scalable, AI-enabled platforms today will gain stronger operational control tomorrow.
Therefore, forward-looking investment is not simply a technology decision. It is a strategic move toward resilient, data-driven healthcare growth.
Conclusion
Enterprise hospital management systems are no longer back-office tools. They define how hospitals control costs, protect compliance, and scale operations with confidence. Therefore, investing in the right architecture today determines how well an organization performs tomorrow.
With structured governance, strong interoperability, and AI-enabled intelligence, growth becomes manageable. Intellivon helps healthcare enterprises build systems that strengthen operations while enabling long-term, measurable performance.
Build an Enterprise-Grade Hospital Management System With Intellivon
At Intellivon, enterprise hospital management systems are engineered as regulated healthcare infrastructure, not as administrative software layered onto fragmented hospital tools.
Our approach ensures clinical workflows, revenue cycles, inventory systems, and analytics operate within one governed framework. Organizations retain control over access policies, integration standards, and financial reporting without introducing fragmentation or regulatory exposure.
Why Partner With Intellivon?
- Enterprise-grade hospital management architecture designed for multi-site healthcare networks
- Proven delivery across complex EHR ecosystems and expanding hospital groups
- Compliance-by-design framework with embedded audit trails and role-based governance
- Secure, interoperable infrastructure supporting cloud, hybrid, and on-prem deployment models
- AI-enabled operational intelligence with a measurable efficiency and financial performance focus
Book a strategy session with Intellivon to design a hospital management system that strengthens governance, improves operational efficiency, and supports sustainable enterprise growth.
FAQs
Q1. What is an enterprise-grade hospital management system?
A1. An enterprise-grade hospital management system is a scalable digital platform that manages clinical operations, revenue cycles, compliance, and reporting across one or multiple hospital entities.
It integrates with EHRs, payers, labs, and external systems using secure data standards. In addition, it embeds audit controls and governance frameworks from the start. Therefore, it supports both operational efficiency and regulatory readiness.
Q2 How is an enterprise HMS different from basic hospital software?
A2. Basic hospital software often supports a single facility and focuses on departmental tasks. In contrast, an enterprise HMS is designed for multi-hospital networks with centralized governance.
It includes real-time dashboards, interoperability layers, compliance automation, and scalable architecture. As a result, it supports expansion, mergers, and value-based care models without system redesign.
Q3. How much does it cost to build an enterprise hospital management system?
A3. The cost typically ranges between $50,000 and $150,000, depending on scope, integrations, and compliance requirements. Factors such as multi-site deployment, interoperability complexity, and security controls influence pricing.
In addition, ongoing maintenance usually accounts for 15 to 20% annually. Therefore, long-term ROI depends on structured architecture and phased implementation.
Q4. Why is interoperability important in hospital management systems?
A4. Interoperability allows hospital systems to exchange structured data with EHRs, insurers, laboratories, and health information exchanges. Without it, manual reconciliation and reporting errors increase.
Therefore, standardized integration using HL7 and FHIR improves data consistency. In addition, it strengthens care coordination and revenue accuracy across departments.
Q5. When should a hospital upgrade to an enterprise-grade HMS?
A5. Hospitals should consider upgrading when they expand across locations, face revenue leakage, struggle with compliance audits, or lack real-time operational visibility. In addition, mergers and value-based reimbursement models often require stronger governance controls.
Therefore, an enterprise-grade platform becomes essential when operational complexity exceeds what legacy systems can manage.






