Hospital operations rely on constant movement across departments, facilities, and systems. However, these signals rarely come together into a single operational view. In large, multi-site healthcare organizations, data is scattered across EHRs, workforce systems, financial platforms, and manual reporting layers. This forces leadership teams to reconcile numbers before taking action. When visibility is broken, decisions take longer, margins shrink, and operational risk rises.
Enterprise-grade hospital operations management software provides structure to this complexity by combining clinical, operational, and financial data into a unified control layer. It standardizes KPIs across facilities, separates real-time monitoring from finalized reporting, and adds governance directly into workflows. Operations leaders gain early insight into bottlenecks. Finance teams view performance without needing validation cycles, and compliance stakeholders maintain traceable oversight.
At Intellivon, we design these systems as strong enterprise infrastructure intended to scale, integrate, and stay resilient under regulatory and operational pressure. In this guide, we explain how we build systems that reliably scale, integrate with existing ecosystems, and support long-term operational resilience.
Why You Should Invest In Operations Management Software
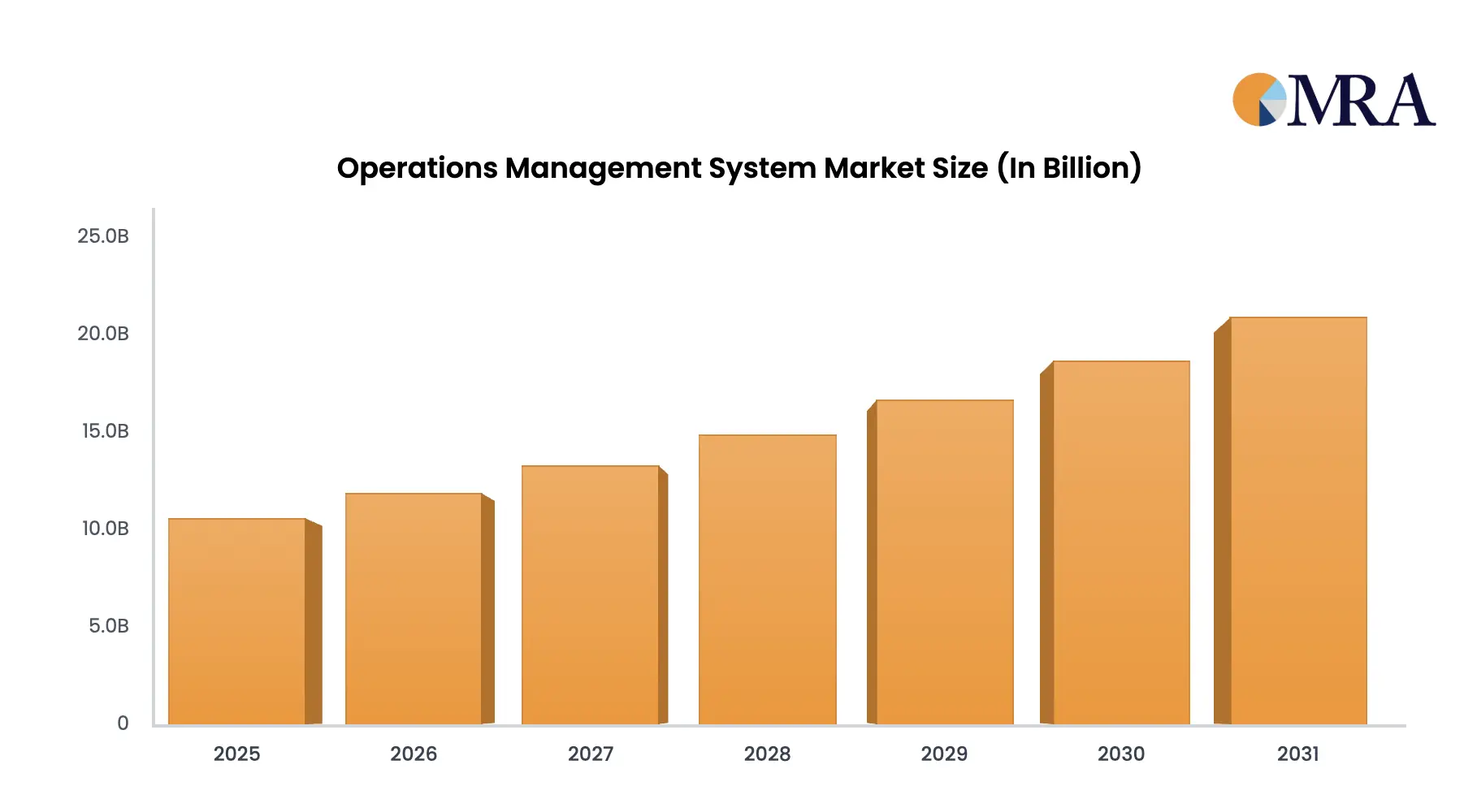
Operations management software (OMS) improves workflow coordination, resource allocation, and operational decision-making across large enterprises. The global OMS market is currently valued at nearly $50 billion and is projected to grow at a 12% compound annual growth rate (CAGR) through 2033.
Within healthcare, the focus is more specialized. Hospital operations platforms increasingly prioritize EHR integration, interoperability, and advanced analytics to manage clinical and financial performance together. This healthcare-specific segment is expected to reach approximately $15 billion in 2025 and expand to nearly $45 billion by 2033, also growing at a projected 12% CAGR.
These growth patterns reflect a broader shift. Healthcare organizations are no longer investing in standalone workflow tools. Instead, they are building integrated operational control systems that connect clinical care, workforce management, and financial performance under a unified architecture.
Market Insights:
- Accelerated digital transformation and demand for real-time visibility to support faster, data-driven operational decisions.
- Growing adoption of AI and machine learning to automate workflows, strengthen supply chain resilience, and enable cloud-based scalability.
- In healthcare, expansion is driven by EHR integration, patient engagement platforms, revenue cycle optimization, and the operational pressures of aging populations.
Why Invest In OMS Now
Investing in hospital operations management software delivers measurable returns at a time when healthcare enterprises face sustained cost pressure and operational strain.
Organizations that implement integrated digital operations report 25–50% reductions in operational costs by streamlining workflows, improving resource utilization, and eliminating waste, which directly increases throughput capacity.
Research also shows that digital systems enhance information quality and real-time visibility, leading to better decision-making, improved productivity, and lower error rates.
At a broader industry level, AI and advanced analytics are projected to generate $200–$360 billion in annual net savings across healthcare through automation, optimization, and cost control. re.
What Is A Hospital Operations Management Software?
Hospital operations management software is a system that helps hospitals run their daily operations in a coordinated and organized way. It connects different departments and tools, such as electronic health records, staff scheduling systems, bed management, operating room scheduling, supply chain tracking, and billing platforms, into one shared operational view.
Instead of relying on separate reports from different systems, leaders can see what is happening across the hospital in real time. They can track patient flow, staff availability, room usage, and service performance without manually comparing spreadsheets or reconciling numbers.
For large hospitals and multi-site health systems, this software acts as a central control layer. It brings operational data together, standardizes key performance measures, and supports faster, more informed decisions. When built correctly, it helps reduce delays, improve resource use, and maintain clear oversight across departments while keeping reporting accurate and compliant.
How An OMS Works
Hospital operations management software (OMS) works by connecting day-to-day hospital activity into one operational system. It pulls signals from clinical, staffing, scheduling, supply chain, and financial tools, then turns them into a shared view leaders can act on.
The goal is simple, which is fewer blind spots, faster decisions, and tighter control across departments and sites.
1. Connect hospital data sources
An OMS integrates with systems like the EHR, staffing tools, OR scheduling, bed management, supply chain, and billing. It creates a single operational view without replacing what already works.
2. Standardize metrics and definitions
The platform aligns KPI definitions across facilities and departments. This prevents teams from reporting different numbers for the same metric, which reduces confusion and delays.
3. Process data in real time and in batches
Operational signals like bed status or staffing levels are updated in near real time. Financial and compliance reporting can run on reconciled data to stay accurate and audit-ready.
4. Trigger workflows and task coordination
When bottlenecks appear, the OMS routes tasks to the right teams. For example, it can flag delayed discharges, bed turnover delays, or staffing gaps and assign actions.
5. Deliver role-based dashboards
Each role sees what they need. Operations leaders track throughput, unit leaders track capacity, and executives see system-wide performance without manual report validation.
6. Improve with analytics and forecasting
Over time, the OMS identifies patterns. It can support forecasting for demand, staffing, and capacity, so teams can plan instead of reacting.
A hospital OMS works best when it functions as a shared operational layer, not just a dashboard. When data, workflows, and governance sit in one system, hospitals can improve throughput, reduce delays, and protect margins at enterprise scale.
The Hospital Problems This Software Solves
Hospitals rarely fail because of a single breakdown. Instead, performance suffers when disconnected systems, delayed reporting, and manual coordination slow down decision-making.
As patient volumes rise and reimbursement pressures increase, operational gaps quickly translate into financial strain. Hospital operations management software addresses these systemic issues by connecting workflows, standardizing visibility, and improving execution across departments.
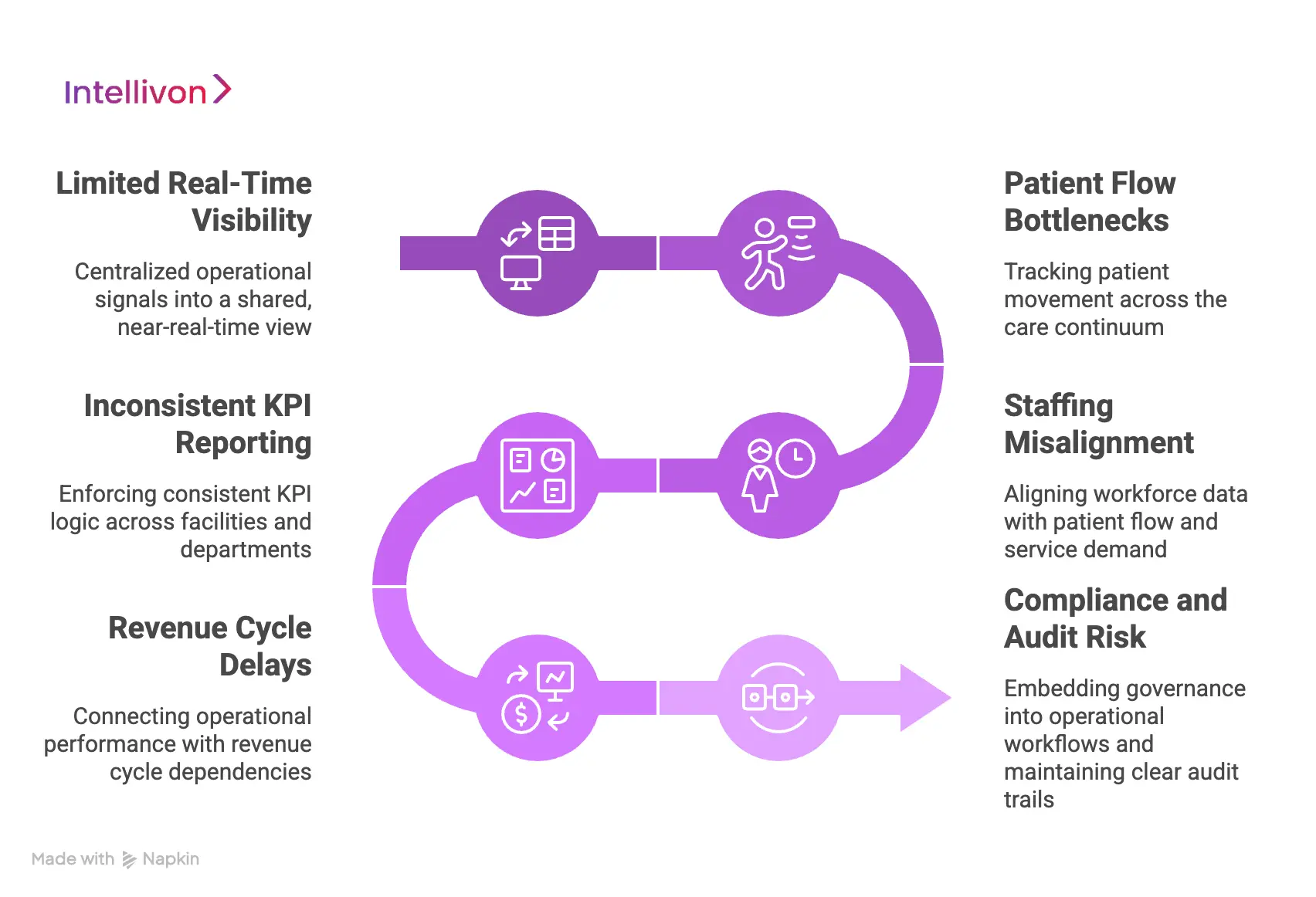
1. Limited Real-Time Visibility
In many hospitals, operational data sits across multiple systems that do not communicate effectively. Leaders rely on static dashboards or manually compiled reports that lag behind live activity.
As a result, bottlenecks are identified late, and corrective action is delayed. An OMS centralizes operational signals into a shared, near-real-time view. This enables faster escalation, quicker intervention, and more confident decision-making across service lines.
2. Patient Flow Bottlenecks
Bed assignment delays, discharge coordination gaps, and inefficient transfers reduce capacity even when physical resources exist. These bottlenecks increase wait times, extend the length of stay, and limit revenue opportunities.
An OMS tracks patient movement across the care continuum. By identifying constraints early, hospitals can improve throughput and free up capacity without expanding infrastructure.
3. Staffing Misalignment
Staffing schedules often fail to reflect real-time patient acuity and demand fluctuations. This results in overtime costs, agency dependency, and staff fatigue. Over time, burnout and turnover increase operating expenses further.
An OMS aligns workforce data with patient flow and service demand. This supports smarter scheduling decisions and better cost control while maintaining quality of care.
4. Inconsistent KPI Reporting
Departments may calculate performance metrics differently, leading to conflicting reports at the executive level.
Leaders spend time validating numbers instead of acting on insights. Without standardized definitions, accountability becomes unclear. An OMS enforces consistent KPI logic across facilities and departments. This creates a reliable source of truth that supports strategic planning and operational governance.
5. Revenue Cycle Delays
Operational breakdowns often impact documentation accuracy, coding timelines, and billing submission. When clinical and financial workflows operate separately, reimbursement cycles slow, and denial rates increase.
An OMS connects operational performance with revenue cycle dependencies. This reduces lag between care delivery and reimbursement while improving financial predictability.
6. Compliance and Audit Risk
Regulatory reporting requires consistent data definitions and traceable records. Fragmented systems make it difficult to demonstrate control during audits.
Manual reconciliation increases the risk of reporting errors. An OMS embeds governance into operational workflows and maintains clear audit trails. This strengthens compliance readiness across regions and reduces exposure to penalties.
When these structural problems persist, hospitals operate reactively and absorb avoidable cost pressure. A well-architected operations management system restores control, aligns teams around consistent data, and supports sustainable performance at enterprise scale.

Architecture Of A Hospital Operations Management Software
Enterprise hospital operations management software is not a single application layer. It is a governed operations platform that can run across multiple hospitals, service lines, and regions without losing performance, auditability, or control.
The architecture must support high-volume events, multi-system interoperability, strict access controls, and consistent KPI logic across sites.
1. Enterprise Integration and Interoperability Layer
This layer connects the OMS to EHRs, ADT feeds, OR systems, workforce platforms, supply chain, RCM, and analytics environments. It supports APIs, HL7/FHIR where applicable, and event-based interfaces for real-time signals.
It also manages partner and vendor connectivity so integrations remain stable during upgrades and system changes.
2. Identity, Access, and Data Segmentation Layer
Enterprise hospitals need fine-grained control over what each role can view and act on. This layer enforces role-based access, facility-level segmentation, and jurisdiction-aware policies where required.
It supports audit logging, traceable access history, and least-privilege visibility to reduce compliance exposure.
3. Operational Data Platform Layer
This is the foundation that stores and organizes operational data. It includes a governed data lake or warehouse, curated operational marts, and standardized operational data models.
It also supports patient identity matching and cross-system record linking, so operational metrics remain accurate across sites and systems.
4. Metric and Semantic KPI Layer
This is where enterprise control is won or lost. The OMS needs a canonical KPI layer that defines how occupancy, throughput, utilization, LOS drivers, staffing ratios, and turnaround times are calculated.
It supports versioning, approvals, and change control so KPI definitions remain consistent across departments and reporting cycles.
5. Real-Time Event and Stream Processing Layer
Enterprise OMS platforms require live signals for capacity, patient flow, bed status, transport, staffing gaps, and OR changes. This layer processes event streams, applies operational rules, and generates alerts with low latency.
It also isolates real-time operational views from reconciled reporting to prevent “live noise” from corrupting executive metrics.
6. Workflow Orchestration and Decision Layer
This layer turns insights into action. It triggers tasks, routes escalations, and coordinates cross-team workflows such as discharge readiness, bed turnover, transfer approval, staffing reallocation, and supply exceptions.
It also supports rule engines and configurable pathways so enterprises can adapt workflows without rebuilding the platform.
7. Reporting, Visualization, and Command Center Layer
This layer delivers role-based views across the organization. Unit leaders see operational execution, command centers monitor system-wide flow, and executives track enterprise KPIs with drilldowns.
It supports dashboards, alerts, and operational playbooks, while maintaining consistent metric definitions through the semantic layer.
7. Observability, Reliability, and Audit Layer
Enterprise platforms must be measurable and resilient. This layer provides data lineage, pipeline monitoring, uptime controls, error handling, and performance tracing.
It also maintains audit-ready histories for KPI changes, workflow actions, and data transformations, supporting investigations and regulatory reviews.
8. AI Enablement Layer
At enterprise scale, AI must be controlled, not bolted on. This layer supports forecasting for demand and staffing, bottleneck prediction, anomaly detection, and operational recommendations.
It includes guardrails such as explainability, validation, and human oversight so automation remains safe, defensible, and trusted.
An enterprise OMS architecture succeeds when it delivers operational speed without sacrificing governance. It creates a stable foundation that hospitals can scale across sites, integrate with changing ecosystems, and run under real operational pressure with full executive control.
Data & Integrations For Hospital Operations Management Software
Hospital operations management software is only as strong as the data that feeds it. In large healthcare enterprises, operational signals come from many systems that were never designed to work as one. If integrations are shallow or inconsistent, leaders receive partial visibility and unreliable metrics.
A well-architected OMS depends on structured data pipelines, governed integrations, and consistent data definitions across the enterprise.
1. Core Clinical Systems
An OMS must integrate with the hospital’s Electronic Health Record (EHR) and ADT feeds. These systems provide patient movement, admission status, discharge timing, and clinical activity signals. Without accurate clinical data, patient flow tracking and capacity planning break down.
Integration must support near real-time updates where required. At the same time, it must preserve reconciled reporting logic for financial and compliance use cases.
2. Workforce & Staffing Systems
Staffing platforms provide schedules, shift allocations, overtime data, and skill mix information. When connected to patient volume and acuity signals, this data supports smarter staffing decisions.
Enterprise OMS platforms align workforce data with operational demand rather than viewing staffing in isolation.
3. Bed Management & Patient Flow Tools
Bed tracking systems, transport coordination tools, and transfer platforms generate critical throughput signals. These integrations allow hospitals to monitor bottlenecks in real time.
Without this layer, discharge delays and transfer gaps remain hidden until performance declines.
4. Supply Chain & Asset Systems
Supply chain platforms provide inventory levels, equipment availability, and procurement timelines. When integrated into OMS, they help prevent operational slowdowns caused by shortages or equipment constraints.
This is especially important for multi-site networks managing shared resources.
5. Revenue Cycle & Financial Systems
Operational performance directly affects billing accuracy and reimbursement timelines. Integrating revenue cycle systems ensures that clinical documentation, coding, and billing workflows remain aligned.
This reduces denial risk and shortens payment cycles.
6. Data Standardization & Governance
Raw data from multiple systems often uses different formats and definitions. A mature OMS includes a data standardization layer that aligns terminology, validates inputs, and enforces consistent KPI logic.
It also embeds audit logging, access control, and change tracking to maintain compliance and reporting integrity.
7. Secure, Scalable Integration Architecture
Enterprise hospitals require secure APIs, event-driven integrations, and scalable data pipelines. The integration layer must handle high transaction volumes without performance degradation.
It should also remain stable during vendor upgrades or system changes.
When data and integrations are governed correctly, hospital operations management software becomes a reliable control layer rather than a reporting overlay. Clean pipelines, standardized definitions, and resilient integrations ensure that leaders can trust the numbers they act on across departments, facilities, and regions.
Features Of A Hospital Operations Management Software
Hospital operations management software must support execution at the unit level while maintaining enterprise oversight. The right features do not simply display performance metrics.
They connect workflows, standardize decision-making, and create measurable operational control across facilities. Below are the capabilities large healthcare systems require to operate efficiently at scale.
1. Real-Time Operational Visibility
An enterprise OMS delivers live insight into patient flow, bed occupancy, staffing levels, transport queues, and service line performance. Instead of waiting for end-of-day reports, leaders see developing bottlenecks as they occur.
This visibility allows faster escalation and coordinated intervention. For example, teams can identify discharge delays before beds become constrained.
Over time, consistent real-time monitoring reduces reactive decision-making and improves throughput reliability across high-volume environments.
2. Centralized Command Center Dashboards
Large hospital networks require system-wide oversight, especially across multiple facilities or regions. Command center dashboards aggregate operational data into one governed enterprise view.
Executives can monitor KPIs such as capacity utilization, turnaround times, and departmental performance without reconciling separate reports.
These dashboards typically include:
- Enterprise-wide occupancy and throughput metrics
- Facility-level performance comparisons
- Escalation indicators and risk flags
This structure improves coordination between local teams and enterprise leadership.
3. Patient Flow & Capacity Management
Patient movement across admission, transfer, and discharge directly affects revenue and care quality. An OMS tracks flow across units and highlights delays in bed assignment, transport coordination, or discharge readiness.
The system provides structured visibility into length-of-stay drivers and capacity constraints. It can also surface patterns that contribute to congestion during peak periods.
With clearer flow management, hospitals increase available capacity without expanding infrastructure.
4. Workforce Optimization
Staffing costs represent a significant portion of hospital operating expenses. An OMS connects scheduling systems with real-time patient volume and acuity signals.
This allows leaders to adjust coverage based on demand rather than fixed schedules. It also reduces dependency on overtime and agency staffing.
Workforce optimization features often include:
- Skill mix alignment tracking
- Shift coverage alerts
- Overtime trend monitoring
These controls improve financial stability while supporting staff sustainability.
5. Workflow Automation & Task Coordination
Operational delays often occur because responsibilities are unclear or communication is fragmented. An OMS includes rule-based task routing that assigns actions when thresholds are reached.
For example, discharge tasks can be triggered automatically when clinical criteria are met. Bed turnover teams can receive alerts when room readiness falls behind targets.
This reduces manual coordination and ensures accountability across teams.
6. Standardized KPI & Reporting Layer
Enterprise hospitals require consistent metric definitions across facilities and departments. An OMS includes a centralized KPI framework that aligns performance reporting.
This prevents conflicting numbers at the executive level and reduces time spent validating data. It also supports compliance reporting by maintaining traceable definitions and change history.
A standardized reporting layer strengthens governance and improves strategic planning.
When these features work together within a governed architecture, hospital operations management software becomes a control system rather than a reporting tool. It supports faster decisions, protects margins, and enables scalable operational discipline across complex healthcare environments.

AI in Hospital Operations Software: Where It Helps, Where It Risks
Artificial intelligence can strengthen hospital operations when applied with discipline. It can surface early risk signals, improve forecasting accuracy, and reduce manual coordination. However, AI in enterprise healthcare must remain controlled and explainable. The objective is to improve operational clarity, not automate critical decisions without oversight.
Below is a practical view of where AI adds value and where it introduces risk.
Safe AI Use Cases
AI delivers the most value when it supports operational awareness rather than making irreversible decisions.
- Predict discharge readiness delays: Models can identify patients likely to face discharge barriers based on documentation gaps, pending consults, or care coordination signals. This helps teams intervene earlier and improve throughput.
- Forecast bed demand and staffing strain: AI can analyze historical admission patterns, seasonal trends, and service line performance to anticipate capacity pressure. This supports proactive workforce planning and surge readiness.
- Identify likely OR overruns: Predictive models can flag cases at risk of exceeding scheduled time based on procedure type and historical duration. This allows surgical teams to adjust schedules before delays cascade.
- Detect bottlenecks and recommend queue order: AI can surface congestion points in transport, bed turnover, or discharge workflows. It can suggest prioritization logic while leaving final decisions to operations teams.
These use cases enhance visibility and planning without replacing human judgment.
High-Risk AI Use Cases
AI becomes risky when it directly alters patient pathways or operational decisions without human validation.
- Automatic patient routing across units
- Auto-cancellation of procedures or appointments
- Staffing reallocations executed without leadership approval
- Any system-triggered action that could affect clinical outcomes
In regulated healthcare environments, decisions that influence care delivery require accountable oversight. Fully autonomous operational control introduces legal, ethical, and compliance risk.
AI Governance Requirements
Enterprise hospitals must embed governance into any AI-enabled OMS platform. Key safeguards include:
- Human approval for operational changes
- Clear explanation of model outputs and decision logic
- Comprehensive audit logs for every AI-generated recommendation
- Bias testing and validation against historical performance
- Rollback mechanisms to reverse automated changes
- Continuous performance monitoring of model accuracy
Without these controls, even well-designed AI systems can erode trust.
AI should reduce operational noise, not introduce new risk. When applied carefully, it improves planning and coordination. When applied without governance, it creates instability. In enterprise hospital operations, AI must remain a disciplined support layer within a controlled infrastructure.
How We Build A Hospital Operations Management Software
Enterprise hospital operations platforms fail when teams treat them like workflow apps. At scale, OMS must operate as a governed infrastructure that connects clinical operations, staffing, capacity, supply chain, and financial dependencies without breaking under real production load.
At Intellivon, we build these platforms with a platform-first approach that prioritizes interoperability, metric governance, operational reliability, and audit readiness from day one. Below is our delivery process, designed for large health systems.
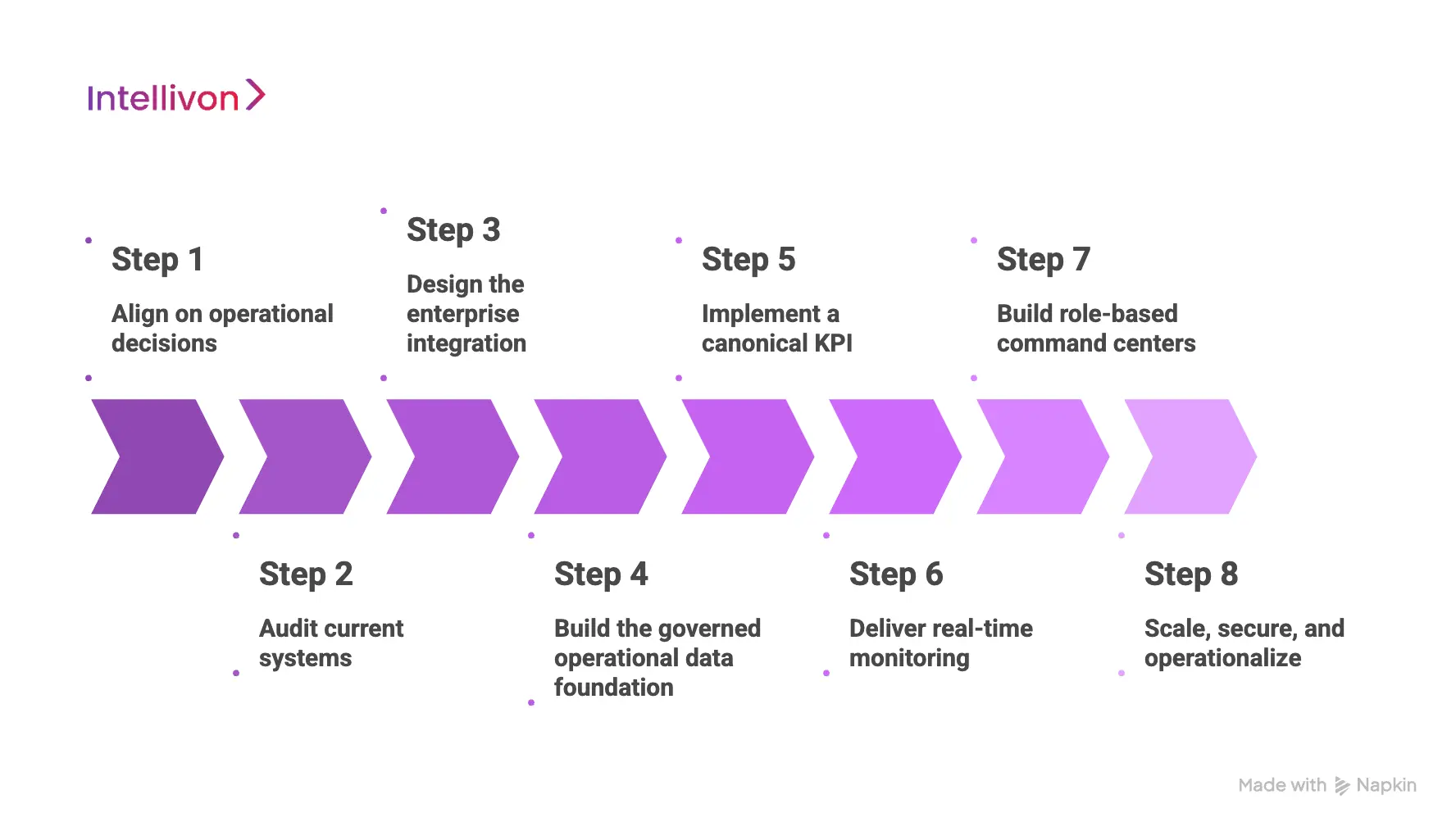
Step 1: Align on operational decisions
We start by mapping the decisions leaders need to make daily, weekly, and monthly. This includes patient flow control, staffing actions, OR utilization, discharge performance, and capacity escalation. We also identify which decisions must be real-time and which require reconciled reporting.
Next, we define who owns each workflow across departments and facilities. This prevents “shared responsibility” from becoming “no accountability.” Finally, we translate decision needs into measurable outcomes and success metrics that leadership can track.
Step 2: Audit current systems
We assess the operational systems already in place and how data moves between them. This includes EHR signals, ADT feeds, staffing tools, bed management systems, supply chain platforms, and RCM dependencies. We identify where work is manual, where metrics conflict, and where latency creates operational blind spots.
We also review how upgrades and vendor changes have impacted integrations in the past. This discovery phase highlights the real constraints that will affect architecture choices. It also prevents building an OMS that looks good in demos but fails in production.
Step 3: Design the enterprise integration
We design an integration approach that fits your ecosystem rather than forcing a rip-and-replace. Depending on the environment, we use APIs, event streams, HL7/FHIR interfaces, and secure connectors to ingest operational signals.
We plan for multi-site scaling and ensure integrations remain stable during EHR upgrades and interface changes. We also define data ownership and synchronization rules so systems do not overwrite each other. Security and access controls are built into integration from the start. The goal is resilient connectivity that survives enterprise complexity.
Step 4: Build the governed operational data foundation
A hospital OMS needs a trusted operational data layer, not scattered extracts. We create a governed data foundation that validates inputs, standardizes terminology, and links records across systems. This often includes operational data marts designed for patient flow, staffing, OR operations, and supply chain visibility.
We also implement data quality checks and exception handling so bad data does not quietly corrupt dashboards. Where required, we support identity matching and cross-facility linking. This foundation ensures leaders see consistent performance signals across departments and sites.
Step 5: Implement a canonical KPI
Most operations platforms fail because every department defines metrics differently. We build a canonical KPI layer that standardizes how key measures are calculated across the enterprise. This includes definitions for occupancy, throughput, turnaround time, bed turnover, discharge delays, staffing ratios, and utilization.
We implement version control, approvals, and change tracking so KPI updates remain auditable. This also allows leadership to compare performance across facilities without reconciliation cycles. When metrics are governed, accountability becomes clearer, and decisions become faster.
Step 6: Deliver real-time monitoring
We separate real-time operational monitoring from reconciled reporting to protect trust. Real-time layers capture signals such as bed status changes, transfers, transport queues, staffing gaps, and OR schedule shifts. We pair these signals with workflow orchestration, so alerts lead to action, not noise.
For example, the platform can flag discharge readiness delays and route tasks to care coordination teams. Thresholds and escalation rules are configurable based on service line needs. This creates operational discipline while keeping teams in control.
Step 7: Build role-based command centers
We design dashboards around what each role needs to do, not what is easy to visualize. Unit leaders get execution views, command centers get system-wide flow control, and executives get reconciled KPI reporting with drilldowns. Access is segmented by role, facility, and service line to maintain governance.
We also build traceable audit paths so leadership can understand where numbers come from. Reporting includes operational trends, variance drivers, and performance comparisons across sites. This improves clarity without creating a dashboard overload problem.
Step 8: Scale, secure, and operationalize
Enterprise OMS platforms must remain stable after go-live, not just during rollout. We implement observability for pipelines, integrations, and workflow performance so issues are detected early.
We also support monitoring, rollback plans, and structured release management so that change does not introduce operational instability. Security controls include access enforcement, audit logs, and policy-based visibility.
If AI capabilities are introduced, we apply governance with human approvals and explainability. The end result is an OMS that scales across facilities, adapts to change, and remains reliable under real operational pressure.
Cost To Build A Hospitals Operations Management Software
At Intellivon, digital health wallet apps are built as a regulated healthcare financial infrastructure, not as payment features layered onto existing systems. The focus stays on creating platforms that operate safely across providers, payers, regions, and evolving financial regulations. Every design decision accounts for governance, interoperability, and long-term risk exposure from the start.
When budget constraints exist, scope is refined with intent. However, security controls, consent enforcement, settlement logic, and auditability are never reduced. Therefore, enterprises avoid remediation costs that surface after launch. Predictability replaces rework, and long-term ROI remains protected.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Operational Assessment | Workflow mapping, stakeholder alignment, KPI identification, systems audit | $12,000 – $20,000 |
| Enterprise Architecture Design | Integration strategy, data models, workflow orchestration logic | $15,000 – $28,000 |
| Integration & Interoperability Layer | EHR, staffing, ADT, bed management, supply chain, RCM integrations | $25,000 – $45,000 |
| Operational Data Platform | Data normalization, validation, KPI standardization, identity matching | $20,000 – $38,000 |
| Real-Time Monitoring & Workflow Engine | Event processing, alerting, task routing, escalation logic | $18,000 – $32,000 |
| Command Center & Role-Based Dashboards | Executive views, unit dashboards, facility comparisons | $15,000 – $28,000 |
| Security & Governance Controls | Access control, audit trails, policy enforcement, and compliance mapping | $14,000 – $24,000 |
| Testing & Enterprise Validation | Performance testing, integration testing, security review, compliance checks | $10,000 – $18,000 |
| Deployment & Scalability Readiness | Cloud/hybrid deployment, observability setup, performance tuning | $12,000 – $20,000 |
Total initial investment: $141,000 – $253,000
Ongoing maintenance and optimization: 15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-scoped digital health wallet programs face pressure when indirect cost drivers are ignored. Planning for these early protects budgets, timelines, and compliance posture as transaction volume grows.
- Integration complexity increases as EHRs, claims systems, and payer rules expand
- Compliance overhead grows due to audits, financial reporting, and regulation updates
- Governance requires continuous policy tuning, consent reviews, and exception handling
- Infrastructure costs rise with transaction volume, analytics, and monitoring workloads
- Change management includes onboarding finance, operations, and support teams
- Continuous monitoring becomes critical as financial scrutiny increases
Best Practices to Avoid Budget Overruns
Based on Intellivon’s experience delivering enterprise healthcare and fintech platforms, these practices consistently lead to controlled costs and predictable outcomes.
- Start with a clearly defined wallet model before expanding programs or regions
- Embed governance, auditability, and financial controls into core architecture
- Use modular components that scale without redesign
- Plan interoperability early to avoid expensive retrofitting
- Maintain observability across performance, fraud, and compliance
- Design for regulatory evolution rather than one-time certification
Request a tailored proposal from Intellivon’s healthcare and fintech experts to receive a delivery roadmap aligned with your budget constraints, compliance exposure, and long-term digital health wallet strategy.
Conclusion
Hospital operations management software is no longer a departmental tool. It is enterprise infrastructure that determines how efficiently care is delivered and how reliably margins are protected. When workflows, staffing, capacity, and revenue dependencies operate in silos, performance gaps widen.
A well-architected OMS brings these moving parts into a governed, real-time operational layer. It standardizes metrics, strengthens oversight, and enables faster intervention without compromising compliance.
For large health systems, the goal is not visibility alone. It is disciplined execution at scale. With the right foundation, operational complexity becomes measurable, manageable, and financially sustainable across facilities and regions.
Build A Hospital Operations Management Software With Intellivon
At Intellivon, hospital operations management platforms are built as enterprise operational infrastructure, not as workflow overlays layered onto fragmented hospital systems. Every architectural and delivery decision prioritizes interoperability, KPI governance, real-time reliability, and regulatory control. This ensures operations platforms function consistently across facilities, departments, and regions, not just during initial rollout.
As health systems expand service lines, add facilities, or modernize their EHR ecosystems, operational complexity increases. Stability becomes critical. Throughput monitoring, staffing alignment, workflow orchestration, and executive reporting must remain accurate under production load. Organizations retain control over performance metrics, operational rules, and compliance requirements without introducing data conflicts, integration fragility, or reporting inconsistencies.
Why Partner With Intellivon?
- Enterprise-grade operational architecture designed for multi-site, regulated healthcare environments
- Proven delivery across large provider networks with complex integration landscapes
- KPI governance framework that standardizes performance definitions across facilities
- Real-time and reconciled reporting pipelines built with separation and audit control
- Secure, modular infrastructure supporting cloud, hybrid, and on-prem deployments
- AI-enabled operational forecasting and optimization with human oversight and traceability
Book a strategy call to explore how Intellivon can help you design and scale a hospital operations management platform with confidence, control, and long-term enterprise resilience.
FAQs
Q1. What is hospital operations management software?
A1. Hospital operations management software is an enterprise platform that connects patient flow, staffing, scheduling, supply chain, and revenue cycle systems into one coordinated operational layer. It provides real-time visibility and standardized performance metrics across facilities. This allows leadership teams to monitor throughput, manage capacity, and reduce operational delays without reconciling fragmented reports.
Q2. How does hospital operations management software improve ROI?
A2. OMS improves ROI by reducing length of stay, increasing bed utilization, optimizing staffing levels, and accelerating reimbursement cycles. Even small improvements in throughput or overtime reduction can significantly impact margins at scale. By standardizing KPIs and improving decision speed, enterprises reduce waste and protect long-term financial performance.
Q3. How long does it take to build hospital operations management software?
A3. For large health systems, development typically takes 6 to 12 months, depending on integration complexity and scope. Multi-site environments with extensive EHR, staffing, and RCM integrations may require phased implementation. A structured architecture and governance plan reduces delays and protects timelines.
Q4. Does hospital operations management software integrate with EHR systems?
A4. Yes. Enterprise OMS platforms integrate with EHRs, ADT feeds, workforce systems, bed management tools, supply chain platforms, and financial systems. Secure APIs and event-driven integrations ensure operational signals remain accurate and synchronized across departments without disrupting existing workflows.
Q5. Is AI necessary in hospital operations management software?
A5. AI is not mandatory, but it can enhance forecasting and bottleneck detection when properly governed. Safe use cases include demand prediction and staffing strain alerts. However, AI must include human oversight, audit trails, and explainability to prevent operational and compliance risk in regulated healthcare environments.





