The most fragile phase of care rarely occurs inside the hospital. It begins after a patient is discharged, when instructions are shared, and systems move on. However, recovery rarely follows a linear path once the patient returns home. This is where small gaps quietly turn into preventable complications.
Healthcare enterprises experience this disconnect daily. Teams work hard to ensure safe discharge, yet governance often ends too early. As a result, care delivery becomes fragmented beyond institutional boundaries. Programs such as the Transition of Care model (TOC) implemented at UC San Diego Health show how this gap can be addressed through structured post-discharge oversight rather than ad-hoc follow-ups.
At Intellivon, we design enterprise-grade tele-transition platforms that work with existing systems rather than replacing them. Our approach preserves legacy data, respects established workflows, and integrates cleanly across EHRs, analytics, and operational infrastructure. This experience shapes the perspective shared throughout this blog, where we explain how these platforms are built from the ground up to scale safely, remain compliant, and deliver long-term operational impact.
Key Takeaways Of The Tele-Transition Market
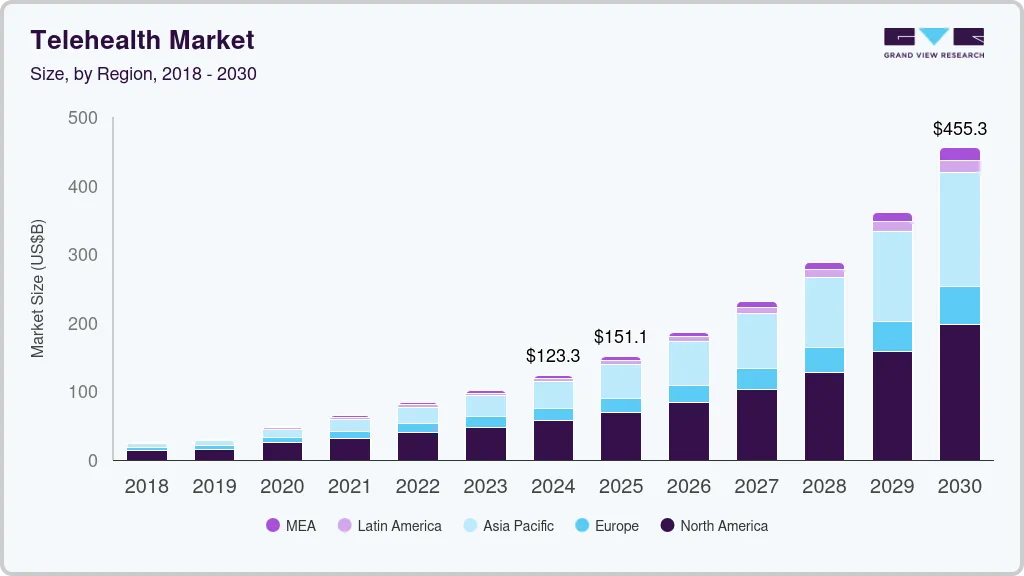
Telehealth has moved well beyond early adoption. The global market stood at roughly USD 123 billion in 2024 and is forecast to more than triple to about USD 455 billion by 2030, reflecting a sustained annual growth rate of around 24.7 percent.
Market Insights:
- Global telehealth and virtual care markets are expanding at an estimated 24–32% CAGR through 2030, making them among the fastest-growing healthcare segments.
- Growth is driven by three forces: rising chronic disease prevalence, sustained acceptance of virtual care by patients and clinicians, and increasingly supportive reimbursement structures.
- In parallel, hospital economics are being reshaped by readmission penalties and value-based initiatives such as the CMS Hospital Readmissions Reduction Program (HRRP).
- These programs directly tie reimbursement to 30-day post-discharge outcomes, accelerating investment in post-acute and transition-of-care virtual models.
Where Tele-Transition Platforms Sit in the Value Chain
- Today, tele-transition capabilities are typically embedded within broader telehealth or virtual care service lines.
- The services segment accounts for more than 45% of total virtual care revenue, reinforcing a service-led delivery model rather than a platform-first one.
- Most enterprises currently assemble TOC workflows by stitching together EHRs, telehealth tools, RPM platforms, and care management systems.
- This fragmented architecture creates a strategic gap for integrated tele-transition platforms purpose-built around readmission reduction and post-acute performance.
Buyer Segments and Use Cases
- Primary buyers include large health systems, IDNs, ACOs, and payviders operating under risk-bearing or value-based contracts.
- For these organizations, outcomes within the first 7 to 30 days post-discharge have a direct and measurable impact on revenue and margin.
- Core use cases include: Virtual transition-of-care clinics following inpatient discharge, Emergency department transition-of-care (ED-TOC) programs, Post-surgical virtual follow-up pathways, and Medication-focused post-discharge telehealth for chronic conditions
- Conditions such as heart failure are common entry points due to high readmission rates and reimbursement sensitivity.
As virtual care scales, ownership of the post-discharge window is becoming a defining differentiator. Tele-transition platforms are where clinical continuity and financial performance now converge.
What Is a Tele-Transition Platform?
A tele-transition platform is a digital care layer designed to manage patients during the period immediately after hospital or emergency department discharge. This window is clinically fragile and operationally complex. Without structure, small issues often escalate into readmissions or avoidable complications.
Unlike standard telehealth tools, tele-transition platforms focus on continuity rather than episodic visits. They coordinate post-discharge outreach, virtual follow-ups, medication reconciliation, and care navigation within defined timeframes. As a result, care teams maintain visibility even after the patient leaves the facility.
These platforms integrate directly with existing clinical and operational systems. They pull discharge signals from EHRs, route patients into appropriate virtual workflows, and document outcomes in an auditable manner. This ensures accountability without disrupting legacy infrastructure.
How Does It Work?
A tele-transition platform runs like a governed post-discharge workflow. It starts the moment a discharge event is recorded and continues until the patient is stabilized and handed back to longitudinal care. Each step has a clear owner, a defined timeline, and auditable documentation. As a result, follow-up becomes predictable instead of reactive.
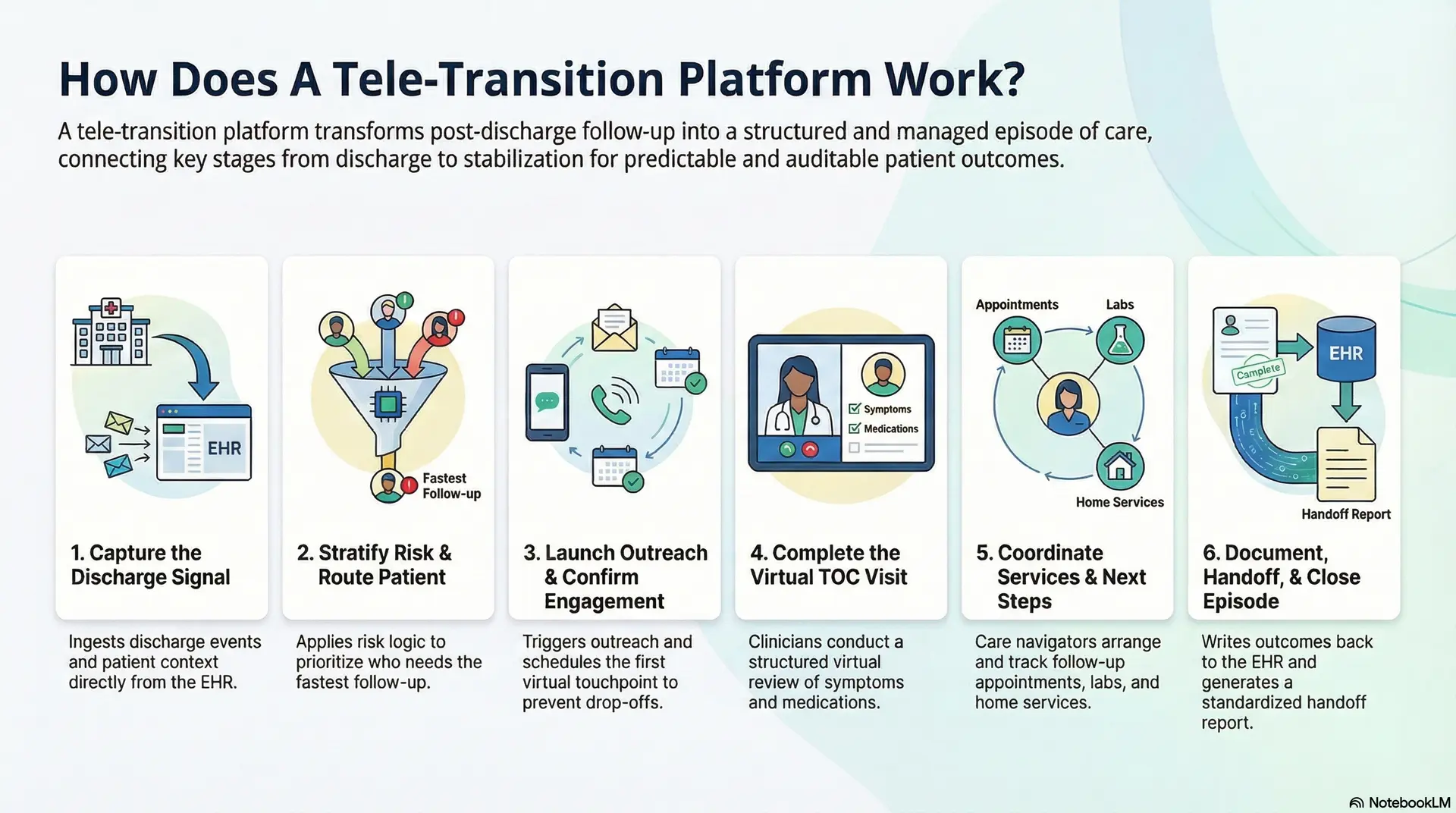
1) Capture the discharge signal
The platform ingests discharge events from the EHR and related systems. It pulls context such as diagnosis, meds, labs, and disposition. This creates a reliable starting point for outreach and clinical review.
2) Stratify risk and route the patient
Next, the platform applies risk logic to prioritize who needs fast follow-up. It can use scoring models, rules, or cohort definitions set by the enterprise. Based on risk, the patient is routed into the right pathway and timeline.
3) Launch outreach and confirm engagement
The system triggers outreach through approved channels and schedules the first virtual touchpoint. If the patient does not respond, the platform runs escalations. This prevents silent drop-offs after discharge.
4) Complete the virtual TOC visit
Clinicians conduct a structured virtual review focused on symptoms, meds, and warning signs. They reconcile medications, clarify instructions, and resolve barriers to adherence. When needed, they order follow-ups or escalate care safely.
5) Coordinate services and next steps
Care navigators arrange PCP or specialist follow-ups, labs, imaging, or home services. The platform tracks completion, not just referral creation. This keeps the plan actionable and measurable.
6) Document, hand off, and close the episode
Finally, the platform writes back outcomes to the EHR and generates a standardized handoff. It closes the TOC episode once milestones are met or risk resolves. This creates accountability and clean reporting for value-based programs.
Tele-transition platforms work because they treat discharge as a managed episode, not a single event. They connect signals, outreach, clinical review, and handoffs into one governed flow, which reduces downstream surprises.
What Is UCSD’s TOC Model?
UCSD’s Transition of Care model is a hospitalist-led virtual program focused on the period immediately after discharge. Patients receive structured virtual follow-up to review symptoms, medications, and next steps. The model prioritizes early intervention and clear handoffs back to primary care.
In practice, it reduced 30-day readmissions from 20.1% to 14.9%, with the strongest impact among moderate-risk patients at UC San Diego Health.
How Does UCSD’s TOC Model Stand Out?
UCSD’s Transition of Care model stands out because it treats post-discharge care as a defined clinical phase, not a courtesy follow-up. The model applies structure, ownership, and timing to a window where risk is highest. As a result, outcomes improve without adding unnecessary operational burden.
1. Hospitalist-led accountability
The program is led by hospitalists who understand the inpatient context. This ensures continuity between discharge decisions and post-discharge follow-up. Clinical accountability remains clear throughout the transition window.
2. Early, time-bound intervention
Patients are contacted quickly after discharge. Virtual visits happen before issues escalate. This timing is critical for preventing avoidable readmissions.
3. Structured virtual workflows
Visits follow a standardized framework focused on symptoms, medications, and care gaps. This consistency improves quality and reduces variation across patients and providers.
4. Targeted risk focus
The model concentrates resources on moderate-risk patients, where early action delivers the highest return. This avoids over-serving low-risk cases while intervening before high-risk escalation.
5. Clean handoffs to longitudinal care
Each episode ends with a documented handoff back to primary or specialty care. This closes the loop and preserves continuity beyond the TOC window.
UCSD’s model succeeds because it combines clinical ownership, disciplined timing, and structured workflows. At UC San Diego Health, transition of care is managed as an operational system, not an informal follow-up process.
Why the Post-Discharge Window Is the Highest-Risk Period in Care Delivery
The period immediately after discharge is one of the most volatile phases in healthcare delivery. Clinical responsibility shifts, patient behavior changes, and oversight drop sharply. However, medical risk does not decline at the same pace. This mismatch is why avoidable complications and readmissions concentrate in the first few weeks after discharge.
Health systems see the impact clearly in utilization data. Many downstream events originate from gaps that surface days after patients return home. This window demands structured attention, not passive follow-up.
1. Clinical Risk Spikes After Discharge
Studies show that nearly 20% of patients experience an adverse event within weeks of discharge. Many of these events involve medication errors, unmanaged symptoms, or delayed follow-up. Importantly, a significant portion is considered preventable with earlier intervention.
Once patients leave a controlled setting, care becomes fragmented. Without timely review, small issues escalate into emergency visits or readmissions.
2. Readmissions Cluster in the First 30 Days
Across major conditions, 18–21% of patients are readmitted within 30 days of discharge. For high-volume diagnoses such as heart failure and pneumonia, the risk is even higher. Early readmissions often signal breakdowns in care continuity rather than treatment failure.
From an enterprise perspective, this timing aligns directly with financial penalties and value-based performance metrics.
3. Medication and Follow-Up Gaps Drive Escalation
Medication changes are common at discharge and frequently misunderstood. Research shows that nearly one in five post-discharge adverse events is medication-related. Missed follow-ups further compound this risk.
Patients who see a clinician within 7 days of discharge consistently show lower readmission rates. When that visit does not happen, deterioration often goes unnoticed.
4. Operational Ownership Ends Too Early
Discharge workflows often conclude once instructions are delivered. At that point, accountability becomes diffused across teams and systems. No single function owns the outcome during the recovery phase.
This lack of ownership explains why post-discharge risk persists despite strong inpatient care.
The post-discharge window concentrates clinical, operational, and financial risk into a short timeframe. Enterprises that treat this phase as a governed care episode, rather than a handoff, are best positioned to reduce avoidable utilization and stabilize outcomes.
TOC Models Reduce Readmissions to 14.9% From 20.1%
Reducing readmissions is not about adding more follow-ups. It is about controlling the period immediately after discharge, when patient risk peaks. During this window, accountability often fades. When transition-of-care models are structured correctly, they deliver measurable clinical and financial impact quickly.
Evidence from large health systems confirms this shift. These outcomes are operational and repeatable. More importantly, they align directly with enterprise priorities around utilization control and value-based performance.
What the UC San Diego VToC Model Demonstrates
At UC San Diego Health, a hospitalist-led Virtual Transition of Care clinic is focused on early post-discharge intervention. Patients received structured virtual follow-ups soon after leaving the hospital. These visits addressed medication issues, symptom changes, and next-step planning before escalation.
The results were significant. Thirty-day readmission rates declined from 20.1% in benchmark patients to 14.9% among those enrolled in the VToC program. This reduction reflects a material shift in downstream utilization, not a marginal gain.
Why Moderate-Risk Patients Showed the Strongest Gains
The largest improvements appeared in moderate-risk patients. This group included individuals with LACE+ scores between 50 and 75. These patients are stable enough for discharge but vulnerable to deterioration without timely support.
Traditional care models often miss this window. Low-risk patients receive unnecessary attention, while high-risk patients escalate quickly. TOC platforms concentrate resources where early intervention delivers the highest return, improving outcomes and cost efficiency together.
Structured transition-of-care models demonstrate measurable reductions in readmissions within standard reporting windows. For enterprises operating under value-based pressure, this impact makes TOC platforms a strategic priority rather than an optional add-on.
Use Cases Of Tele-Transition Platforms Like UCSD
Tele-transition platforms are not built for a single workflow. They support multiple post-discharge scenarios where early intervention changes outcomes. Each use case focuses on a short, high-risk window where structure and accountability matter most. When applied correctly, these platforms improve continuity without adding operational friction.
Below are the most common enterprise use cases modeled on programs such as those implemented at UC San Diego Health.
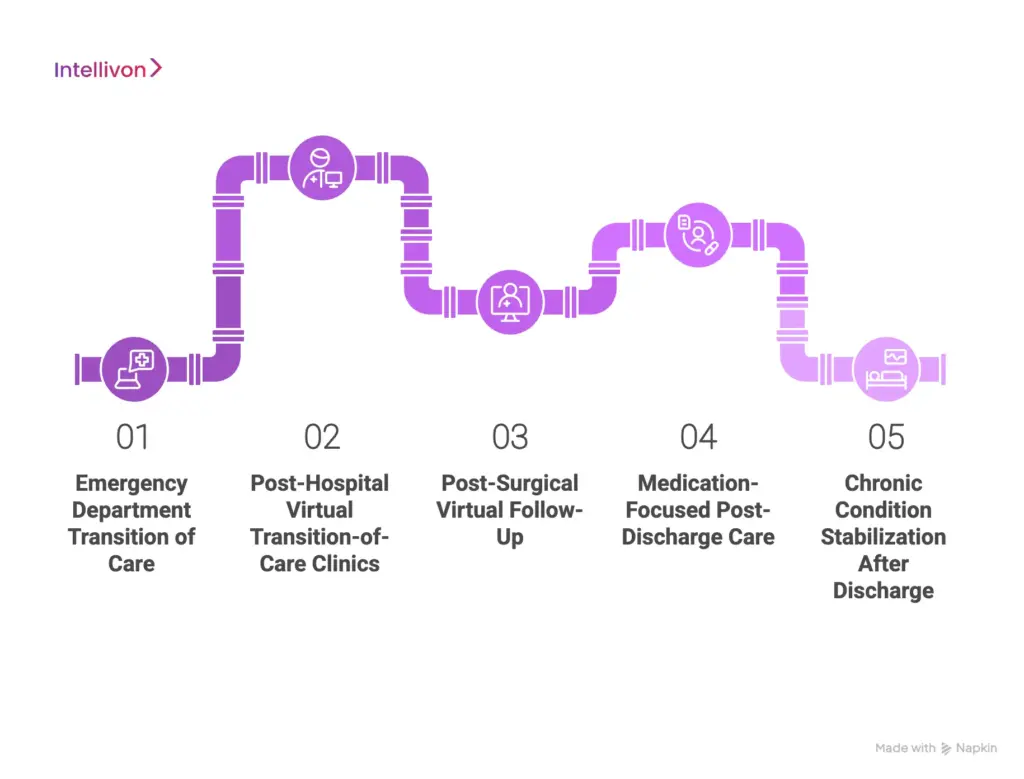
1. Emergency Department Transition of Care (ED-TOC)
Patients discharged from the emergency department often leave without follow-up certainty. ED-TOC programs provide rapid virtual check-ins within days of discharge.
Clinicians review symptoms, medications, and warning signs early. This prevents unnecessary return visits and stabilizes patients before issues escalate.
2. Post-Hospital Virtual Transition-of-Care Clinics
After inpatient discharge, patients face the highest readmission risk within 7 to 30 days. Virtual TOC clinics offer structured follow-up during this window.
Hospitalists or advanced practitioners address care gaps and coordinate next steps. This model consistently reduces 30-day readmissions.
3. Post-Surgical Virtual Follow-Up
Surgical patients often struggle with pain control, wound care, and medication adherence at home. Tele-transition platforms enable early virtual reviews after discharge.
Care teams identify complications sooner and reinforce recovery instructions. As a result, avoidable ED visits decline.
4. Medication-Focused Post-Discharge Care
Medication changes are a leading cause of post-discharge complications. Tele-transition workflows prioritize medication reconciliation and education.
Clinicians confirm understanding, correct errors, and address side effects early. This use case is especially effective for cardiac and chronic disease patients.
5. Chronic Condition Stabilization After Discharge
Patients with heart failure, COPD, or diabetes often deteriorate soon after discharge. Tele-transition platforms support close virtual monitoring and follow-up during early recovery.
Care teams intervene before symptoms worsen. This reduces readmissions while supporting value-based care goals.
Tele-transition platforms apply the same core capability across multiple scenarios. They bring structure, timing, and ownership to the post-discharge window. For enterprises, these use cases represent some of the highest-impact opportunities in virtual care today.
Core Components of a Tele-Transition Platform Like UCSD TOC
A tele-transition platform must function as enterprise infrastructure, not an overlay on virtual care. It needs to support scale, clinical accountability, and governance during the most fragile phase of care delivery. Programs modeled after UC San Diego Health succeed because these components work together as a single operating system.
Each component below is essential for stability, adoption, and long-term impact.
1. Discharge Signal Ingestion
The platform must detect discharge events the moment they occur. This includes inpatient and emergency department discharges across facilities. It also captures the full clinical context, such as diagnoses, medication changes, labs, and discharge instructions.
Without this capability, enrollment becomes manual and inconsistent. At enterprise scale, delayed or partial context leads to missed follow-ups and clinical blind spots. Real-time ingestion ensures post-discharge care begins with accuracy rather than assumptions.
2. Risk Stratification and Cohort-Based Routing
Not every discharged patient carries the same level of risk. The platform must apply structured logic to identify who needs immediate attention and who can follow a lighter pathway. This may include clinical risk scores, utilization history, or enterprise-defined criteria.
This component protects program economics. It ensures care teams focus on patients where early intervention prevents escalation. Without stratification, TOC programs become resource-heavy and difficult to sustain.
3. Standardized Virtual TOC Workflows
Virtual TOC visits must follow defined clinical workflows. These workflows guide providers through symptom assessment, medication reconciliation, and escalation decisions. They also standardize documentation and ensure required steps are never skipped.
Consistency matters at scale. Structured workflows reduce variation across providers while preserving clinical judgment. They also support audit readiness and measurable performance across service lines.
4. Post-Discharge Service Coordination
Preventing readmissions requires more than a single virtual visit. The platform must coordinate downstream actions such as primary care follow-ups, specialty referrals, labs, imaging, or home services. Each action needs tracking through completion.
This component closes the gap between planning and execution. Many post-discharge failures occur because referrals are placed but never completed. Active coordination ensures care plans translate into real-world follow-through.
5. Enterprise Integration and Data Continuity
A tele-transition platform must integrate into existing enterprise systems without disruption. It should write outcomes back to the EHR, analytics platforms, and reporting layers. Legacy workflows and data structures must remain intact.
This integration determines adoption. Platforms that create duplicate records or parallel workflows introduce friction and resistance. Seamless data continuity allows teams to operate within familiar systems while gaining new capabilities.
6. Governance and Performance Reporting
Every TOC interaction must be documented, auditable, and reportable. The platform must support compliance, billing separation, and outcome measurement across populations. Leaders need visibility into utilization, readmissions, and program effectiveness.
Governance sustains the program long term. Without it, reporting breaks down and leadership confidence erodes. Strong governance turns TOC from a pilot initiative into a durable enterprise capability.
Tele-transition platforms succeed when these components operate as a unified system. Together, they transform discharge from an endpoint into a governed care episode. For enterprises, this architecture enables scale, accountability, and measurable post-discharge impact without disrupting existing infrastructure.
Advanced AI Features Of A Tele-Transition Platform Like UCSD TOC
Once a tele-transition platform is operationally stable, AI becomes an accelerant rather than a dependency. In mature enterprise programs, AI is applied selectively to improve timing, prioritization, and consistency across the post-discharge window. Models inspired by programs such as those at UC San Diego Health show how AI can strengthen outcomes without introducing clinical risk.
These capabilities work best when embedded inside governed workflows.
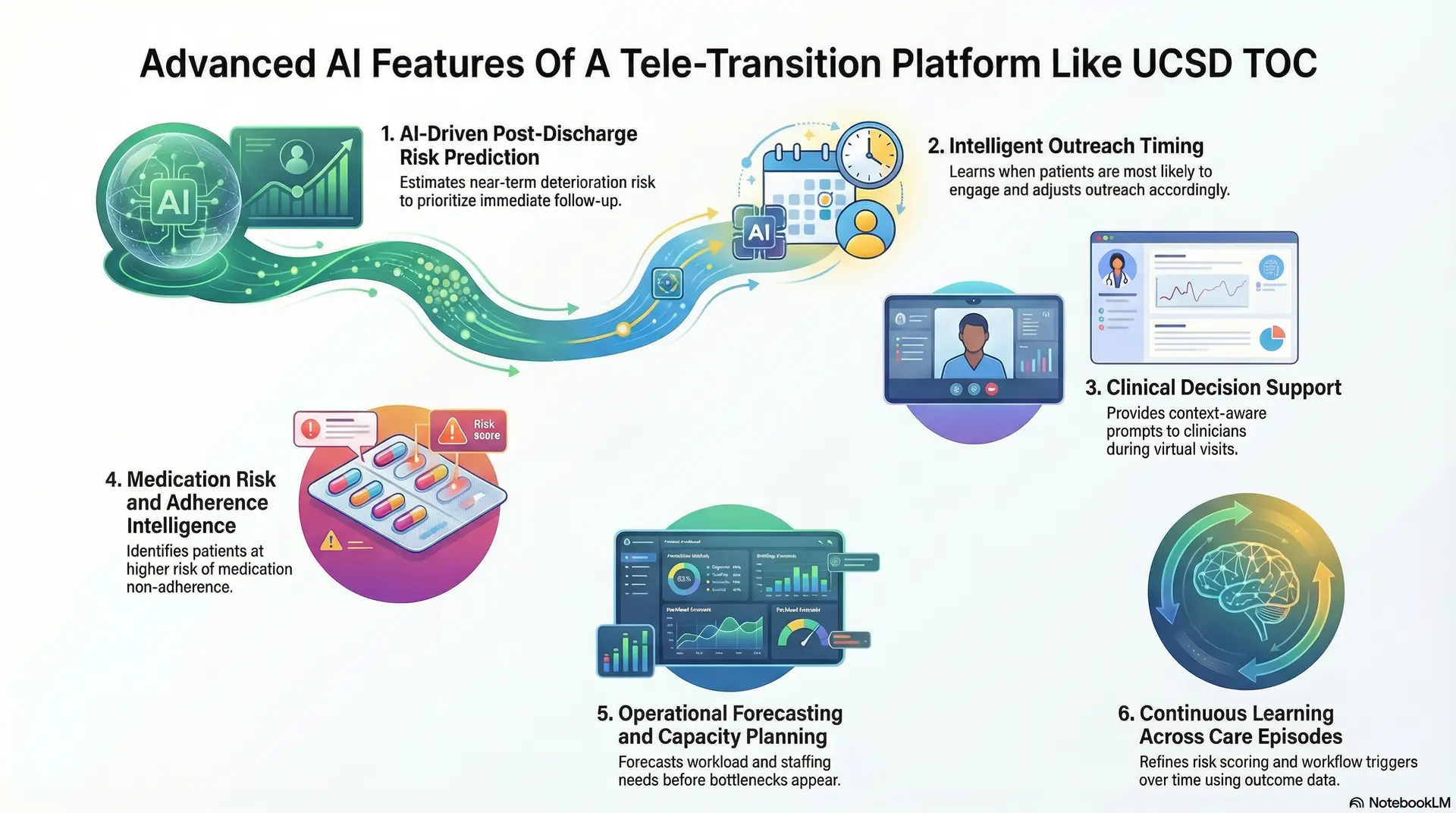
1. AI-Driven Post-Discharge Risk Prediction
AI models analyze discharge summaries, diagnosis history, prior utilization, and recent clinical signals to estimate near-term deterioration risk. The focus is on the first 7 to 30 days after discharge, when escalation is most likely. Predictions help teams decide who needs immediate follow-up and who can safely wait.
This shifts decision-making from static rules to adaptive prioritization. For enterprises, it improves focus without increasing staffing or visit volume.
2. Intelligent Outreach Timing
Not all patients respond to outreach in the same way. AI learns when patients are most likely to engage after discharge and adjusts outreach timing accordingly. If contact attempts fail, escalation rules trigger alternate channels or human follow-up.
This reduces silent disengagement. Care teams spend less time chasing non-responsive patients and more time resolving active risk.
3. Clinical Decision Support
During virtual TOC visits, AI provides context-aware prompts rather than directives. These prompts surface medication conflicts, unresolved discharge instructions, missing follow-ups, or symptom patterns that warrant closer review. Clinicians remain in control of all decisions.
This support improves consistency across providers. It also reduces cognitive load during high-volume transition clinics.
4. Medication Risk and Adherence Intelligence
Medication changes are common at discharge and often misunderstood. AI models identify patients at higher risk of non-adherence by analyzing regimen complexity, prior refill behavior, and documented confusion. These signals guide focused medication review.
Addressing these risks early prevents escalation. For enterprises, this capability directly targets one of the most common drivers of readmissions.
5. Operational Forecasting and Capacity Planning
AI analyzes discharge trends, risk distribution, and follow-up demand to forecast workload across TOC programs. Leaders gain early visibility into staffing needs and clinic capacity requirements. Adjustments can be made before bottlenecks appear.
This supports predictable operations. It also aligns TOC programs with enterprise financial planning.
6. Continuous Learning Across Care Episodes
Each completed TOC episode feeds outcome data back into the platform. AI models refine risk scoring, outreach timing, and workflow triggers over time. Learning occurs within defined governance boundaries.
This ensures the platform improves as populations and care models evolve. Enterprises benefit from adaptability without constant manual reconfiguration.
Advanced AI features elevate tele-transition platforms from reactive follow-up systems to proactive care operating layers. When applied with governance and clinical oversight, AI improves focus, timing, and consistency. For enterprises, this is how tele-transition programs scale intelligently without increasing clinical or operational risk.
Core Architecture Of A Tele-Transition Platform Like UCSD TOC
A tele-transition platform must be built as a layered enterprise architecture, not a single monolithic system. Each layer isolates responsibility, reduces operational risk, and allows independent scaling. Programs modeled after approaches used at UC San Diego Health succeed because architecture decisions support clinical workflows rather than constrain them.
This layered model ensures stability, flexibility, and long-term adoption.
1. Integration and Data Ingestion Layer
This layer connects the tele-transition platform to the enterprise ecosystem. It ingests discharge events, patient demographics, diagnoses, medication changes, and care plans from source systems. Timing matters here because delayed ingestion leads to missed follow-ups and blind spots.
The layer also protects legacy systems. Data flows in and out without forcing changes to existing EHR workflows or ownership models. As a result, enterprises can activate TOC programs without re-platforming core systems.
Typical technologies
- HL7 and FHIR APIs
- Mirth Connect
- Redox
- Apache Kafka
- AWS EventBridge
2. Workflow and Orchestration Layer
The orchestration layer governs how post-discharge care actually unfolds. It controls patient routing, outreach timing, escalation rules, and episode closure. Every step is time-bound and role-specific.
This layer transforms policy into execution. It ensures that TOC workflows behave the same way across facilities, service lines, and patient cohorts. Without orchestration, programs rely too heavily on manual coordination and tribal knowledge.
Typical technologies
- Camunda
- Temporal
- Apache Airflow
- AWS Step Functions
- Custom BPM engines
3. Clinical Application Layer
This layer is where care teams interact with the platform. It supports structured virtual TOC visits, medication reconciliation workflows, and standardized documentation. Clinical logic is embedded in workflows, not hardcoded into interfaces.
By separating clinical workflows from infrastructure, this layer allows iteration without disruption. Providers work within guided flows while retaining clinical judgment and autonomy.
Typical technologies
- React or Angular
- FastAPI or Node.js
- SMART on FHIR frameworks
- Secure video SDKs
4. AI and Decision Intelligence Layer
The AI layer analyzes post-discharge risk, engagement patterns, and operational demand. It supports prioritization, clinical prompts, and forecasting without automating decisions. All outputs remain explainable and auditable.
This layer improves timing and focus. Care teams intervene earlier, while leaders gain insight into emerging risk patterns across populations.
Typical technologies
- Python
- TensorFlow
- PyTorch
- XGBoost
- Scikit-learn
- AWS SageMaker
5. Data Management and Analytics Layer
This layer stores TOC episode data, outcomes, and performance metrics. It supports dashboards, reporting, and longitudinal analysis across service lines. Data is structured to support value-based reporting and audit requirements.
By separating analytics from transactional systems, enterprises gain visibility without impacting clinical performance. Leadership can track utilization, readmissions, and program ROI in near real time.
Typical technologies
- PostgreSQL
- Snowflake or BigQuery
- Amazon Redshift
- Looker or Power BI
- Tableau
6. Security, Compliance, and Governance Layer
This layer enforces access control, audit trails, and data protection. It governs who can see what, when, and why. Compliance requirements are embedded into platform behavior rather than enforced manually.
Strong governance ensures the platform can scale across regions and programs without introducing regulatory risk.
Typical technologies
- OAuth 2.0 and OpenID Connect
- HashiCorp Vault
- AWS IAM
- Audit logging frameworks
A tele-transition platform works when architecture supports care delivery instead of working against it. Layered design allows enterprises to scale programs, integrate safely, and adapt over time. This foundation turns transition-of-care from an operational gap into a governed, measurable capability.
How We Develop a Tele-Transition Platform for Enterprise Scale
Enterprise tele-transition programs fail when they are treated like feature builds. Scale requires governance, integration discipline, and operational design from day one.
At Intellivon, we build tele-transition platforms as enterprise operating layers that preserve legacy data, integrate into existing systems, and hold up under audit. Our experts design for adoption across facilities, not just success in one pilot. Below is our eight-step delivery approach.
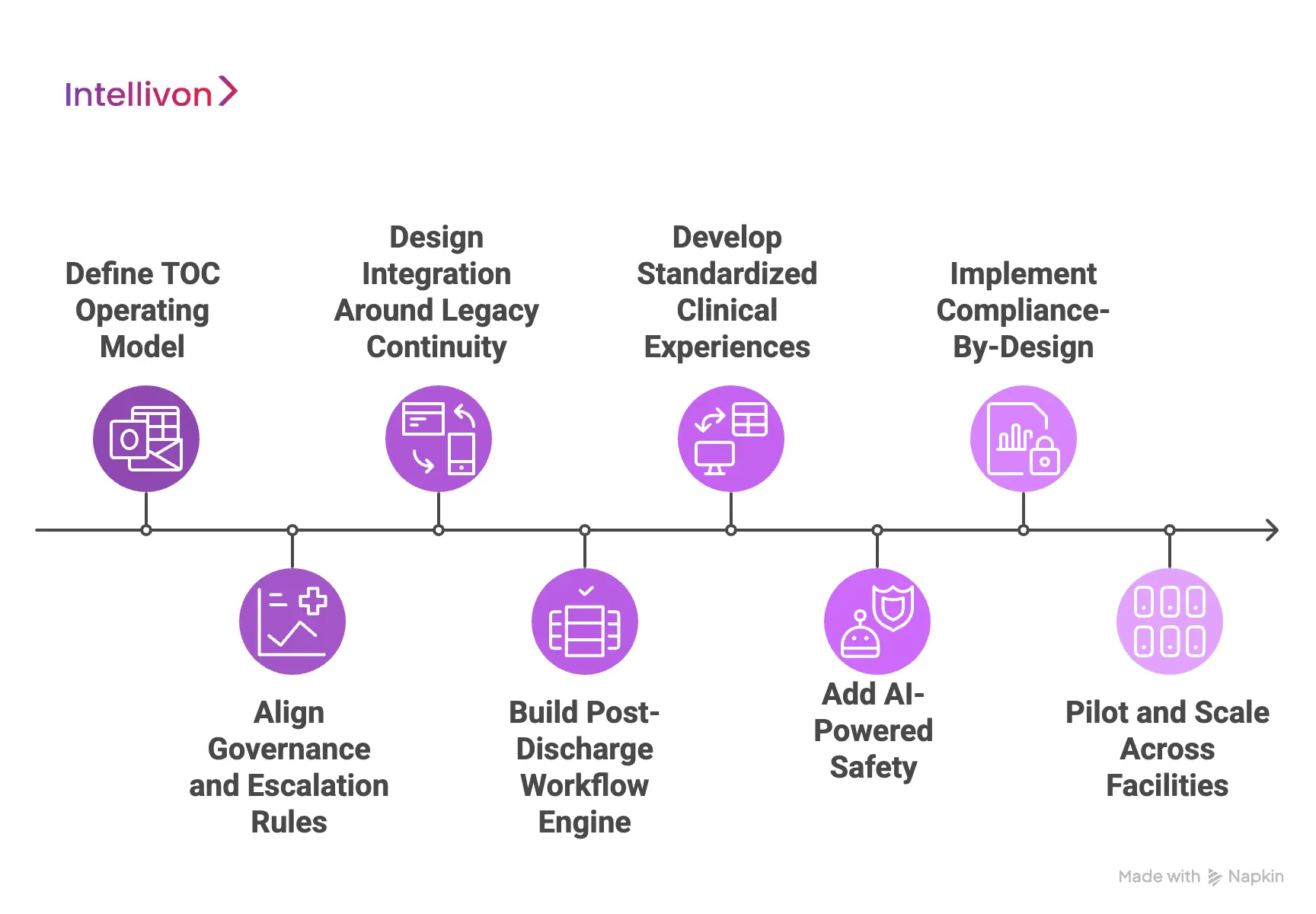
1) Define TOC Operating Model
We begin by mapping how discharge actually works across your system today. Our team documents where risk enters, where ownership drops, and which teams carry post-discharge accountability. We also define which cohorts matter most, such as moderate-risk medical discharges or ED return-risk patients.
This step produces a clear operating model. It establishes who owns each action, what “done” means, and how the TOC episode closes. Without this clarity, platforms become workflow libraries that nobody trusts.
2) Align Governance And Escalation Rules
Next, we lock the clinical boundaries that keep the program safe. We define which clinicians can make which decisions, what triggers escalation, and how handoffs to primary or specialty care are managed. Our experts also standardize documentation requirements so every episode is defensible.
This step protects your organization as volumes grow. It also prevents variation between sites, which is where compliance and outcome drift usually start.
3) Design Integration Around Legacy Continuity
Tele-transition platforms fail when they disrupt the EHR or create parallel records. We design integration as a first-class requirement, not a later sprint. This includes discharge event ingestion, patient context capture, and write-back into the systems your teams already use.
Our approach preserves legacy data models and workflows. Teams gain new capability without learning a new operating reality. This is what drives adoption across service lines and regions.
4) Build Post-Discharge Workflow Engine
We then implement the orchestration layer that governs TOC execution. It controls patient routing, timing, outreach sequences, escalation paths, and episode closure logic. Every step is time-bound, role-aware, and measurable.
This is where tele-transition becomes an operating system. It reduces reliance on manual tracking and removes the need for coordination through spreadsheets and inboxes.
5) Develop Standardized Clinical Experiences
Next, we build the clinical workflows used by hospitalists, navigators, pharmacists, and care coordinators. These flows include symptom review templates, medication reconciliation steps, red-flag prompts, and structured handoff outputs. We keep the experience simple, but we do not remove clinical rigor.
Our experts prioritize usability because adoption depends on it. At the same time, we ensure workflows remain auditable and consistent across providers.
6) Add AI-Powered Safely
AI becomes valuable when it strengthens timing and prioritization. We implement predictive risk scoring, engagement optimization, and context-aware clinical prompts. At the same time, we keep AI advisory, transparent, and governed, so it supports clinicians instead of creating new liability.
We also monitor performance drift. Our team ensures models remain reliable across populations and sites, which is critical in enterprise deployments.
7) Implement Compliance-By-Design
Before scaling, we embed controls that protect the platform. This includes role-based access, consent alignment, audit trails across the TOC episode, and billing-safe documentation separation. We also build reporting that connects operational activity to outcomes, such as readmissions, follow-up completion, and escalation rates.
This step turns TOC into an enterprise program with measurable governance. Leadership gains visibility without manual reporting overhead.
8) Pilot And Scale Across Facilities
Finally, we deploy in a controlled pilot that reflects real operational complexity. We validate workflows, integration reliability, staffing fit, and reporting accuracy. Then we harden the platform based on real usage patterns before expanding across facilities and service lines.
Scaling becomes predictable because the foundation is stable. Our experts support phased rollout planning so adoption grows without compromising clinical control or operational efficiency.
Tele-transition platforms deliver enterprise value when they are built as governed operating layers, not as standalone virtual care tools. Intellivon builds these platforms to integrate seamlessly, preserve legacy continuity, and scale safely across complex health systems.
Clinical and Compliance Requirements Of TOC Platforms
Tele-transition platforms sit at the intersection of clinical decision-making and regulated operations. They manage real patient risk after discharge, often without face-to-face oversight. For enterprises, this means compliance cannot be layered on later. It must be enforced through platform behavior from the first interaction.
The requirements below reflect what regulated health systems actually need to operate TOC programs safely at scale.
1. Defined Clinical Authority and Escalation Boundaries
Every TOC workflow must define who is allowed to make clinical decisions and under what conditions. This includes who can adjust medications, who can escalate care, and when responsibility shifts back to primary or specialty providers.
These rules must be enforced in workflows, not documented in policies alone. Without hard boundaries, platforms expose organizations to scope-of-practice and liability risk.
2. Post-Discharge Clinical Protocol Enforcement
TOC visits must follow enterprise-approved protocols. These protocols define required assessments, medication review steps, and red-flag criteria. The platform should prevent visit completion if the required steps are skipped.
This ensures consistency across providers and locations. It also reduces variation that often leads to adverse events and audit findings.
3. Medication Reconciliation and Attestation Controls
Medication reconciliation is a high-risk activity after discharge. TOC platforms must require explicit confirmation of medication changes, patient understanding, and documented resolution of discrepancies.
Attestation controls matter here. The platform should record who reviewed medications, what was confirmed, and what follow-up was required. This level of detail is often missing in generic telehealth tools.
4. HIPAA-Compliant Identity
TOC platforms must enforce role-based access at a granular level. Clinicians, navigators, and support staff should only see the data required for their role. Session access must be time-bound and auditable.
This is especially critical in post-discharge programs that span multiple teams. Compliance must be technical, not dependent on training or trust.
5. End-to-End Audit Trails
Every action in a TOC episode must be traceable. This includes outreach attempts, missed contacts, clinical reviews, escalations, and handoffs. Audit logs must capture timestamps, actors, and decisions.
These trails protect organizations during regulatory review. They also allow internal teams to investigate outcomes and improve workflows.
6. Billing and Documentation Separation
TOC platforms must support clean separation between inpatient, ED, TOC, and outpatient documentation. Notes, timestamps, and actions must align with the correct billing context.
This requirement is critical under mixed reimbursement models. Without separation, organizations risk duplicate billing, denied claims, or compliance violations.
7. Structured and Verifiable Care Handoffs
Every TOC episode must end with a documented handoff. This handoff should include resolved issues, outstanding risks, and required follow-ups. It must be written back into the EHR in a standardized format.
Verifiable handoffs close clinical responsibility clearly. They also protect downstream teams from acting on incomplete information.
Clinical and compliance requirements determine whether a TOC platform can operate safely beyond pilot scale. When enforcement is built into workflows, enterprises gain control instead of exposure. This is what allows post-discharge care to scale without increasing regulatory or clinical risk.
Common Mistakes When Scaling Tele-Transition Programs
Tele-transition programs often perform well during pilots. However, scaling exposes weaknesses that are invisible at low volume. These failures are rarely clinical. They stem from structural decisions that do not hold up under enterprise load.
Our experience working with large health systems shows that avoiding these mistakes early determines whether TOC becomes a durable capability or a stalled initiative.
1. Tele-Transition as Telehealth Add-On
Many organizations launch tele-transition as an extension of existing telehealth services. In this model, follow-ups rely on informal workflows and disconnected tools. Accountability is implied rather than enforced. As volumes increase, coordination weakens and outcomes plateau.
At Intellivon, we approach tele-transition as an operating layer. Our experts design platforms where post-discharge workflows are governed end-to-end. Ownership, timing, and escalation are enforced by the system, not assumed by teams.
2. Relying on Manual Enrollment and Outreach
A common scaling failure is manual patient identification. Staff review discharge lists, initiate outreach, and track follow-ups by hand. This approach collapses under enterprise volume. Missed patients become routine, and risk accumulates silently.
We eliminate this failure point entirely. Intellivon platforms ingest discharge signals automatically and route patients into TOC workflows without manual intervention. Our teams design for consistency, not heroics.
3. Applying the Same Follow-Up to Every Patient
Enterprises often default to uniform follow-up models. Low-risk patients receive unnecessary attention, while moderate-risk patients do not get enough. Over time, costs rise and clinical impact declines.
Our experts embed risk stratification directly into the platform. Follow-up intensity adjusts based on risk, timing, and context. This ensures resources are applied where early intervention prevents escalation and protects program economics.
4. Stitching Together Fragmented Technology
Many TOC programs rely on loosely connected EHRs, telehealth tools, and care management systems. Data lives in multiple places, and workflows cross system boundaries. As a result, visibility degrades, and reporting becomes unreliable.
At Intellivon, we design for integration from day one. Our platforms preserve legacy systems while creating a unified post-discharge workflow. Data continuity and clean write-back ensure teams operate from a single source of truth.
5. Ignoring Compliance Until After Launch
Some programs focus on speed and defer compliance considerations. Documentation, billing separation, and audit trails are added later. This creates a risk that compounds as the program grows.
We build compliance into platform behavior from the start. Our experts ensure that scope boundaries, documentation standards, and auditability are enforced automatically. This allows enterprises to scale confidently without regulatory surprises.
6. Lacking Clear Episode Closure and Handoffs
Many TOC initiatives fail to define when responsibility ends. Episodes linger without formal closure, and handoffs to longitudinal care are inconsistent. This creates confusion and downstream risk.
Intellivon platforms enforce structured episode closure. Every TOC engagement ends with a documented handoff written back into enterprise systems. Our approach preserves continuity while clearly transferring ownership.
Tele-transition programs fail at scale for predictable reasons. Each mistake reflects a lack of structure, not intent. By designing platforms as governed enterprise systems, Intellivon helps organizations avoid these pitfalls and scale post-discharge care with control, confidence, and measurable impact.
Conclusion
Tele-transition platforms are no longer optional for enterprises managing post-discharge risk at scale. As care delivery extends beyond hospital walls, the ability to govern the first 7 to 30 days after discharge becomes a defining capability. Programs like UCSD’s TOC model show what is possible when structure, accountability, and timing are applied consistently.
For healthcare organizations, the opportunity is not just about reducing readmissions. It is gaining operational control, financial predictability, and clinical continuity across fragmented care journeys. At Intellivon, we build enterprise-grade tele-transition platforms that integrate seamlessly with existing systems and scale without disruption. When built correctly, transition of care becomes a growth enabler, not a cost center.
Build a Tele-Transition Platform With Intellivon
At Intellivon, we build tele-transition platforms as enterprise operating systems, not virtual follow-up tools layered onto discharge workflows. Our platforms are designed to govern how patients move through the post-discharge window, how early risk signals trigger timely intervention, and how accountability is maintained across clinicians, care teams, and regulated enterprise infrastructure.
Each solution is engineered for healthcare organizations operating at scale. Platforms are infrastructure-first and compliance-led, with tele-transition delivered as a governed care phase rather than an informal extension of telehealth. As programs expand across facilities, regions, and value-based contracts, clinical oversight, data continuity, and operational control remain intact.
Why Partner With Intellivon?
- TOC-first platform architecture aligned with post-discharge risk management, readmission reduction, and enterprise governance
- Deep interoperability expertise across EHRs, care management systems, identity platforms, analytics stacks, and billing environments
- Compliance-by-design delivery supporting HIPAA, audit readiness, role-based access, and clean separation from inpatient and outpatient services
- AI-assisted orchestration that prioritizes post-discharge risk, routes follow-up intelligently, and supports clinicians without replacing judgment
- Enterprise delivery model with phased rollout, KPI-driven validation, and controlled scale across service lines and facilities
Talk to Intellivon’s healthcare platform architects to explore how an enterprise-grade tele-transition platform can integrate seamlessly into your existing ecosystem, reduce post-discharge risk, protect regulatory integrity, and scale transition-of-care programs with confidence.
FAQs
Q1. What is a tele-transition platform in healthcare?
A1. A tele-transition platform is a digital care system designed to manage patients during the high-risk period immediately after hospital or emergency department discharge. It coordinates outreach, virtual follow-ups, medication review, and care handoffs. Unlike standard telehealth tools, it governs post-discharge workflows with timing, ownership, and accountability built in.
Q2. How is a tele-transition platform different from regular telehealth?
A2. Telehealth focuses on individual virtual visits. Tele-transition platforms manage an entire post-discharge episode. They control when patients are contacted, how risk is prioritized, and how care is handed back to primary or specialty teams. This makes them suitable for reducing readmissions and supporting value-based care.
Q3. Why are tele-transition platforms important for reducing readmissions?
A3. Most readmissions occur within 7 to 30 days after discharge. During this window, patients face medication confusion, missed follow-ups, and symptom escalation. Tele-transition platforms address these risks early through structured follow-up and coordination, which helps prevent avoidable emergency visits and rehospitalizations.
Q4. Can tele-transition platforms integrate with existing EHR systems?
A4. Yes. Enterprise-grade tele-transition platforms are designed to integrate directly with existing EHRs and analytics systems. They ingest discharge events and write outcomes back without duplicating data or disrupting workflows. This allows organizations to scale programs without replacing legacy infrastructure.
Q5. Who should invest in a tele-transition platform?
A5. Tele-transition platforms are most valuable for large health systems, IDNs, ACOs, and payviders operating under value-based or risk-bearing contracts. Organizations managing high discharge volumes or facing readmission penalties benefit most from owning the post-discharge care window.





