Hospitals and healthcare enterprises are drowning in patient data, yet remain exposed to security gaps. A single system failure can cost millions in downtime, while a breach of protected health information can take years to recover from. Patient data analytics platforms solve this by unifying clinical, financial, and operational data while ensuring HIPAA, GDPR, and FDA compliance, giving decision-makers confidence in both security and insights.
Intellivon has helped global healthcare enterprises build such platforms, turning fragmented systems into secure, audit-ready infrastructures. Our approach integrates encryption, interoperability, resilience, and compliance frameworks into one seamless platform. The result is faster insights, stronger governance, and lower operational risk. This blog will uncover how secure patient data analytics platforms enable healthcare enterprises to thrive, and how we build them from the ground up for long-term success.
Why Security Is the Foundation of Patient Data Analytics
Security in healthcare analytics isn’t optional. It’s essential. In July 2024, a software outage disrupted over 750 U.S. hospitals, knocking out access to fetal monitoring, imaging, and EHR systems, according to a JAMA Network Open study. This proved that downtime is a direct patient-safety risk.
Breaches are also escalating. The Change Healthcare cyberattack compromised the data of 192.7 million individuals, according to the U.S. Department of Health and Human Services HHS OCR breach report. This remains one of the largest exposures of protected health information ever recorded.
What New Rules Expect from Analytics Platforms
Regulators now demand more.
- In February 2024, NIST released SP 800-66r2, a detailed guide for implementing the HIPAA Security Rule, covering safeguards such as risk analysis, transmission security, and audit controls.
- In June 2025, the FDA published its updated Premarket Cybersecurity Guidance, requiring medical devices to include SBOMs, secure development lifecycles, and continuous patching.
Key Principles to Build Security In
- Design for Resilience, Not Just Protection: Outages are inevitable. Build fallback systems like read-only EHR mirrors and cached allergy/medication lists. This reduces harm when live systems stall.
- Harden APIs by Default: ONC reports near-universal hospital support for FHIR APIs and patient-directed access. Secure APIs with scoped tokens, anomaly detection, and rate-limiting. More interoperability means more attack surface.
- Plan for Breach Scenarios: The HHS Change Healthcare report shows that compromise at scale is possible for HHS OCR. Segment PHI zones, enforce least-privilege access, and maintain immutable backups to contain damage.
- Prove Privacy in Use: Peer-reviewed research shows de-identified clinical text has low re-identification risk when stored in secure, governed environments. Platforms should combine de-identification with enclaves and full audit logs to maintain trust.
A secure patient data analytics platforms preserve patient trust and safety. Enterprises must use platforms that can withstand outages, contain breaches, prove compliance, and safeguard privacy by design. Anything less risks both patient outcomes and enterprise credibility.
What Is a Patient Data Analytics Platform?
A patient data analytics platform is a secure, enterprise-grade system that consolidates healthcare data from multiple sources, such as electronic health records (EHRs), connected devices, lab systems, claims, and even mobile health apps, into a unified environment. Instead of leaving information scattered across silos, these platforms transform raw patient data into actionable insights that improve care, streamline operations, and support compliance.
For healthcare organizations, the value lies in using these platforms to not only analyze past events but also predict future risks and prescribe interventions. When security and compliance are embedded from the ground up, enterprises can generate intelligence without compromising patient trust or regulatory standards.
How a Patient Data Analytics Platform Works
1. Data Ingestion and Integration
The platform collects information from diverse sources such as EHRs, wearables, IoMT devices, and billing systems. Advanced integration frameworks standardize these inputs, ensuring data flows seamlessly despite differences in formats or legacy infrastructure.
2. Data Processing and Governance
Once ingested, data undergoes cleaning, normalization, and validation. Governance rules are applied here, such as HIPAA safeguards, access permissions, and audit trails, to ensure every dataset complies with regulatory requirements and enterprise policies.
3. Analytics and Insight Generation
The platform applies descriptive, predictive, and prescriptive analytics. Descriptive analytics review historical patterns, while predictive analytics anticipate risks like readmissions, and prescriptive analytics recommend actions to improve outcomes or reduce costs.
4. Visualization and Enterprise Access
Insights are delivered through secure dashboards and reporting tools tailored to different stakeholders. Role-based access controls ensure that clinical teams, administrators, and executives see only what they are authorized to access, while still benefiting from enterprise-wide intelligence.
5. Continuous Monitoring and Security
Every interaction is monitored in real time. Encryption protects data in motion and at rest, while anomaly detection systems flag irregularities. This proactive approach minimizes breach risks and strengthens system resilience.
This flow ensures enterprises gain actionable insights, regulatory compliance, and operational resilience, the three outcomes healthcare leaders cannot afford to ignore.
Key Takeaways of the Patient Data Analytics Market
With annual growth rates ranging from 15.6% to 22%, this surge is fueled by the rapid expansion of digital healthcare infrastructure, increased adoption of tele-health and mobile health applications, and the exponential growth of data generated from healthcare admissions.
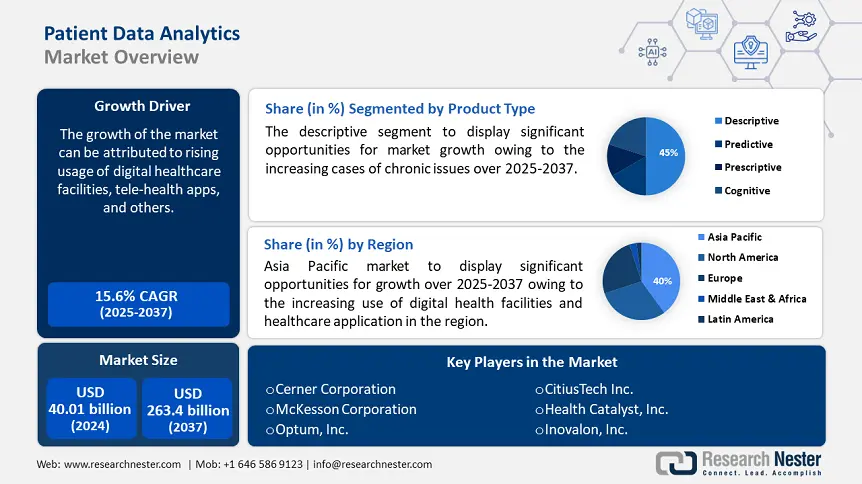
Key Takeaways
- Descriptive analytics currently holds the largest market share, driven by the rising chronic disease burden and the need for historical patient data analysis.
- Predictive and prescriptive analytics are growing rapidly, helping enterprises anticipate risks and optimize care management.
- Financial management applications are expanding, enabling providers and insurers to control costs while improving outcomes.
- Cloud-native and AI-integrated platforms dominate, with over 70% of healthcare institutions using them for real-time insights and collaboration.
- Population health management and personalized medicine are driving innovation and competitive differentiation in the market.
- Partnerships between major technology firms and healthcare providers are accelerating advancements in interoperability and data governance.
North America continues to lead global market share, supported by advanced analytics adoption and significant healthcare digitization. At the same time, emerging economies are posting the highest growth rates as infrastructure strengthens and digital maturity improves.
These shifts highlight how patient data analytics is becoming a transformative force, improving care delivery, enabling cost efficiency, and shaping the future of personalized healthcare worldwide.
Enterprise Use Cases of Secure Patient Data Analytics
A secure patient data analytics platform adapts to different enterprise needs, whether improving outcomes, strengthening compliance, or streamlining operations. Here are the most impactful use cases healthcare organizations are prioritizing.
1. Population Health and Predictive Risk Modeling
By analyzing longitudinal health records and claims data, organizations can identify at-risk populations before conditions escalate. Predictive analytics highlights patients more likely to face complications, supporting proactive interventions that reduce costs and improve care delivery.
2. Remote Patient Monitoring and IoMT Integration
Secure platforms integrate with connected devices such as wearables, glucose trackers, and remote monitoring tools. Real-time data flows allow providers to monitor patients outside clinical walls, reducing avoidable hospitalizations while ensuring safety.
3. Personalized Medicine and Genomics
Integrating genomic and clinical data supports precision medicine strategies, allowing treatments tailored to individual patient profiles. Strong security safeguards ensure compliance when handling highly sensitive genetic datasets.
4. Financial and Fraud Analytics
Analytics extend beyond care delivery into financial operations. Platforms can spot unusual billing patterns, track cost leakage, and minimize fraud or abuse. For insurers and providers alike, this strengthens both compliance and financial resilience.
5. Operational and Resource Optimization
Hospitals and healthcare enterprises use analytics to optimize resource allocation. Forecasting bed occupancy, predicting supply needs, and managing workforce scheduling all reduce waste while improving operational performance.
These use cases highlight how secure analytics platforms deliver value across the healthcare enterprise. They reduce risk, improve efficiency, and help organizations scale responsibly in a highly regulated environment.
Architecture of a Secure Patient Data Analytics Platform
A secure patient data analytics platform relies on a layered architecture where every component plays a role in protecting sensitive information while delivering fast, reliable insights. Security layer is designed into each layer, ensuring that data remains trustworthy from ingestion to visualization.
1. Data Ingestion and Integration Layer
The journey begins at the ingestion layer, where data flows in from electronic health records, connected devices, mobile health apps, and billing systems. At this point, the risk of interception is high, so encryption during transfer is critical.
Standardization frameworks ensure data from different sources can be combined without conflict. Access is carefully managed so that only authorized systems or people can feed information into the platform. This early control builds a strong first line of defense.
2. Storage and Processing Layer
Once inside, the data must be stored securely and made ready for analysis. Encryption at rest shields it even if storage systems are compromised. Sensitive patient records are separated from less critical data to reduce the impact of any breach.
Every action is logged, creating an audit trail that can satisfy regulatory checks or internal investigations. This layer sets the stage for compliance and transparency, making it easier for enterprises to prove governance in real time.
3. Analytics and Intelligence Layer
This is the heart of the platform. After cleansing and normalization, data feeds into descriptive, predictive, and prescriptive analytics models. Descriptive analytics reveal what has already happened, predictive models anticipate risks, and prescriptive insights suggest the best course of action.
Secure environments protect these processes from tampering, while explainability tools ensure leaders can understand how insights are generated. This combination balances innovation with accountability, turning analytics into trusted intelligence rather than opaque outputs.
4. Integration and API Layer
Analytics alone cannot deliver value without integration. This layer connects the platform to hospital systems, insurer databases, and third-party applications. Standards like FHIR and HL7 make interoperability possible, but they also introduce new vulnerabilities.
Token-based authentication, strict permissions, and anomaly detection keep these gateways secure. By safeguarding APIs, enterprises protect the very bridges that allow data to move across ecosystems.
5. Visualization and Access Layer
At the top sits the layer most visible to end users. Dashboards transform analytics into insights tailored for different roles, from clinicians to executives. Security remains central here, like multi-factor authentication verifies identities, while role-based access ensures people see only the information relevant to their responsibilities.
Reports generated in this layer meet HIPAA, GDPR, and other regulatory requirements. In effect, this is where governance meets usability, making analytics accessible without diluting security.
6. Continuous Monitoring and Security Layer
Cutting across all layers is a monitoring framework that never rests. Real-time intrusion detection, vulnerability scanning, and automated alerts ensure the system adapts to evolving threats. Unlike static compliance checklists, this approach treats security as a living function. It reassures enterprises that risks are being managed continuously, not just during annual audits.
Individually, each layer solves a specific challenge. Together, they create a platform that enterprises can trust to handle sensitive patient information without disruption. This architecture not only supports compliance but also enables healthcare leaders to scale analytics confidently, knowing the foundation is both resilient and future-ready.
Features of a Secure Patient Data Analytics Platform
Enterprises cannot afford to treat security as a checklist when building patient data analytics platforms. True security emerges from a set of features that work together to ensure data protection, regulatory compliance, and operational resilience. These features are core capabilities that define whether a platform can be trusted at scale.
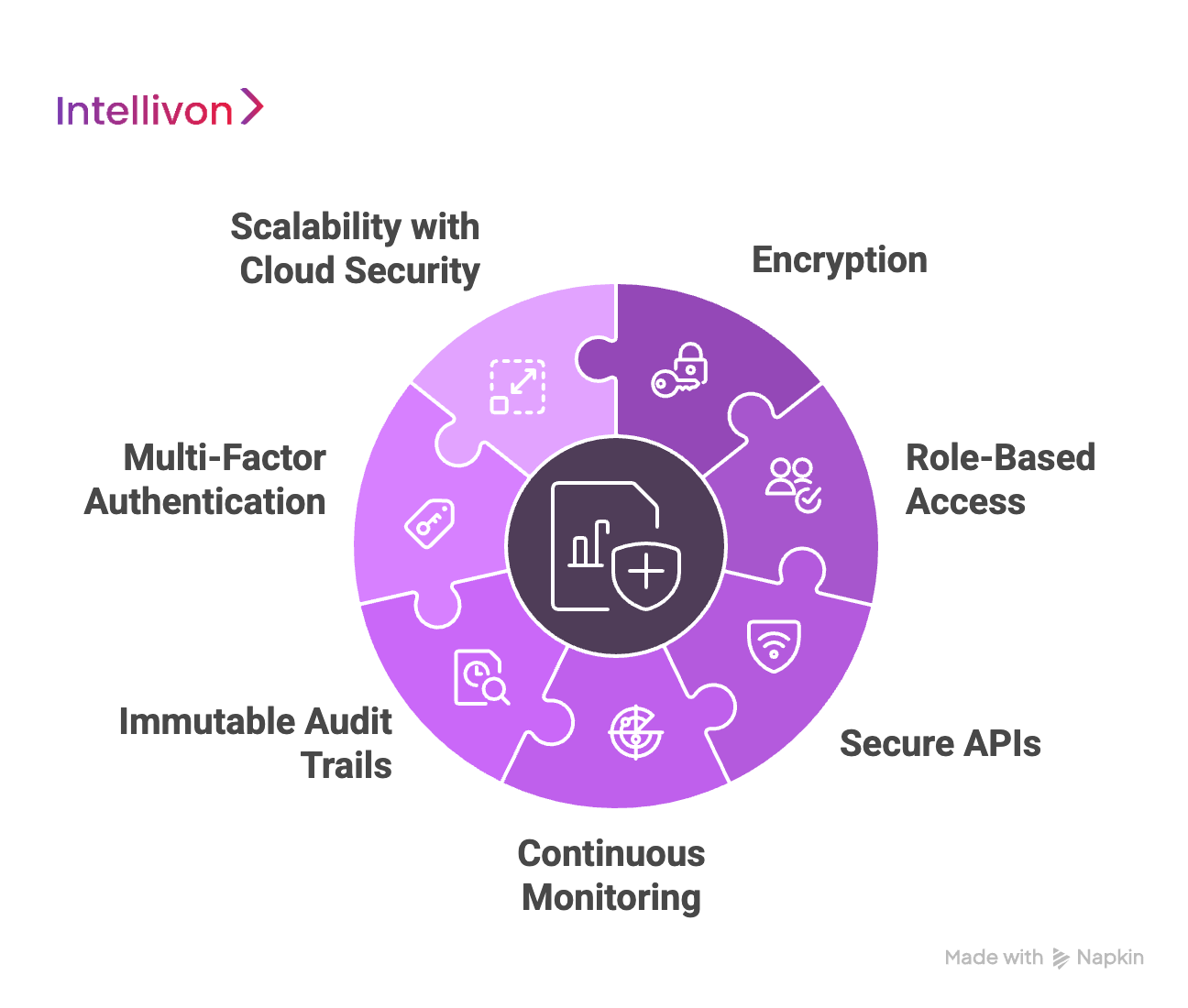
1. Encryption Across the Data Lifecycle
Encryption must protect patient data both when it moves between systems and when it sits in storage. This ensures that even if unauthorized access occurs, the information remains unusable. Enterprises that adopt advanced encryption standards demonstrate to regulators and patients that security is embedded, not improvised.
2. Role-Based Access
Not every user should see every dataset. Role-based access ensures that individuals only view what they need to perform their tasks. When paired with a zero-trust model, where no device or user is inherently trusted, this feature dramatically reduces the risk of insider threats or accidental disclosures.
3. Secure APIs and Interoperability
Modern healthcare depends on interoperability, yet APIs are frequent targets for exploitation. Secure FHIR and HL7 APIs, backed by tokenized authentication and anomaly detection, allow data to flow safely across systems. This balance of openness and security ensures enterprises can collaborate without creating new vulnerabilities.
4. Continuous Monitoring
A static security model is insufficient in today’s environment. Platforms must include continuous monitoring that detects unusual activity, issues alerts, and responds before breaches escalate. This feature turns security from a compliance requirement into a real-time operational safeguard.
5. Immutable Audit Trails
Healthcare enterprises face constant regulatory scrutiny. Immutable logs that record every access, edit, and transfer create a transparent history of activity. These audit trails simplify compliance reporting while also strengthening internal governance. With this feature, enterprises can prove, and not just claim, that they are compliant.
6. Multi-Factor Authentication
At the access layer, identity verification is critical. Multi-factor authentication ensures that stolen passwords alone cannot compromise sensitive information. Combined with device-level verification, this feature fortifies the front door of the platform, reducing one of the most common points of failure.
7. Scalability with Cloud-Native Security
As healthcare data volumes continue to expand, platforms must scale without losing protection. Cloud-native security features, such as container-level controls and automated patching, allow enterprises to expand capacity while keeping pace with new threats. This ensures growth does not come at the expense of trust.
Each feature addresses a different risk, but together they form the foundation of a platform enterprises can trust. From encryption to continuous monitoring, these elements deliver not only regulatory compliance but also the resilience healthcare organizations need to protect patients and accelerate digital transformation.
How to Build a HIPAA-Compliant Patient Data Analytics Platform Step by Step
At Intellivon, our approach to building patient data analytics platforms starts with security and compliance at the foundation. We follow a proven process that balances HIPAA safeguards, enterprise scalability, and healthcare-specific workflows. The result is a platform that is both secure and practical, ready for real-world use.

Step 1: Define Scope and Guardrails
We begin by identifying every source of patient data, like EHRs, IoMT devices, lab systems, and billing platforms. Each dataset is classified according to sensitivity, and access boundaries are set early.
This clarity prevents scope creep and ensures the right protections are applied to the right data. By defining guardrails upfront, enterprises establish a strong security posture before development begins.
Step 2: Run HIPAA-Aligned Risk Analysis
Next, we conduct a risk analysis aligned with NIST 800-66r2 guidance. This involves mapping threats to confidentiality, integrity, and availability of data, and prioritizing them based on impact.
From there, we recommend controls that address those risks directly, such as encryption, access management, and audit logging. The output is a documented risk register that serves as the foundation for compliance and governance.
Step 3: Design Secure Architecture
Our architects then design a layered system that covers ingestion, storage, APIs, and visualization. Security policies, like encryption standards, data segmentation, and logging, are embedded directly into this blueprint.
This ensures the platform is audit-ready before any data moves into production. By designing for security first, enterprises avoid costly redesigns and compliance delays later.
Step 4: Implement Secure Ingestion and Storage
At this stage, we build data pipelines to bring in information from different systems while enforcing encryption in transit. Once inside the platform, sensitive datasets are encrypted at rest and segmented from less critical information.
Access is tightly controlled to minimize exposure. This dual protection guards against both interception and unauthorized use inside the enterprise environment.
Step 5: Apply Privacy and De-Identification Controls
Before analytics can run, patient identifiers are de-identified or pseudonymized. This allows analysts to work with accurate trends while reducing the risk of exposure.
Different datasets are linked with tokens rather than names or IDs, keeping personal details hidden. By combining privacy engineering with security, the platform supports insight generation without putting patients at risk.
Step 6: Harden APIs and External Connections
Healthcare platforms thrive on interoperability, but APIs are common points of attack. We secure FHIR and HL7 endpoints with scoped tokens, strict permissions, and anomaly detection.
Continuous monitoring checks for irregular traffic patterns that may signal abuse. This way, data can flow safely between systems without opening new vulnerabilities.
Step 7: Enable Role-Based Access and Monitoring
We map every user’s access to their roles, ensuring they only see what is necessary. Multi-factor authentication adds another safeguard, confirming identity before access is granted.
Continuous monitoring tools track how users interact with data and flag unusual activity. This balance of trust and vigilance keeps both insiders and outsiders accountable.
Step 8: Prove Compliance and Ensure Resilience
The final step brings together compliance and operational continuity. Immutable audit logs record every transaction, making reporting straightforward during regulatory reviews.
In parallel, failover systems and read-only mirrors keep critical services running even during disruptions. Enterprises can demonstrate compliance with confidence while knowing patient care will not stop if systems encounter an outage.
By following this eight-step process, we help enterprises build secure, resilient platforms that unlock data-driven insights without ever compromising trust, privacy, or regulatory readiness.
Cost Of Building A Compliant Patient Data Analytics Platform
At Intellivon, the goal is to help enterprises build patient data analytics platforms that are both secure and future-ready. That’s why our pricing framework is flexible, aligned with business growth targets, compliance obligations, and clinical priorities, rather than forcing a rigid, one-size-fits-all package.
When initial projections exceed the available budget, the scope is refined collaboratively. The focus always remains on what matters most, which is enterprise-grade reliability, uncompromising security, and regulatory assurance that can withstand HIPAA, GDPR, and global healthcare audits.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Compliance Alignment | Requirement gathering, HIPAA risk modeling, KPI definition, and regulatory scoping (HIPAA, GDPR, FDA) | $6,000 – $12,000 |
| Architecture & Secure Design | Blueprinting layered architecture for ingestion, analytics, governance, and access | $8,000 – $15,000 |
| Data Integration & Normalization | Ingesting EHRs, IoMT device data, lab results, and insurance claims | $10,000 – $20,000 |
| Analytics & Intelligence Layer | Implementing descriptive, predictive, and prescriptive analytics with explainability features | $12,000 – $25,000 |
| Security & Privacy Engineering | Encryption, de-identification pipelines, role-based access, and immutable audit logs | $8,000 – $15,000 |
| Platform Development & Dashboards | Enterprise dashboards, clinical decision support consoles, and compliance reporting tools | $12,000 – $25,000 |
| Testing & Quality Assurance | End-to-end validation, compliance testing, load/stress checks, and resilience validation | $6,000 – $10,000 |
| Deployment & Scaling | Cloud rollout, high-availability configuration, real-time monitoring, and elastic scaling | $6,000 – $12,000 |
Total Initial Investment Range: $50,000 – $150,000
Ongoing Maintenance & Optimization (Annual): 15–20% of initial build cost
Hidden Costs Enterprises Should Plan For
- Integration Complexity: Connecting with legacy EHRs, lab systems, and payer networks often requires additional middleware.
- Compliance Overhead: HIPAA, GDPR, and FDA regulations require ongoing audits, legal support, and continuous updates.
- Data Governance & Curation: Cleaning and managing structured/unstructured datasets add continuous resource needs.
- Cloud Infrastructure Spend: Running large-scale analytics pipelines and real-time dashboards consumes compute if not optimized.
- Change Management: Training clinicians, analysts, and compliance teams on new workflows requires planning and investment.
- Monitoring & Model Drift Prevention: Regular reviews, retraining, and optimization of predictive models prevent compliance and performance gaps.
Best Practices to Avoid Budget Overruns
Drawing from Intellivon’s experience in healthcare, a few practices consistently keep projects on track:
- Start with a Focused Scope: Launch with one department or use case, validate ROI, then expand.
- Design for Compliance Early: Embed HIPAA, GDPR, and FDA safeguards from day one to avoid expensive retrofits.
- Adopt Modular Architecture: Reuse data pipelines, analytics models, and dashboards across new geographies and verticals.
- Optimize Infrastructure Spend: Use cloud-native scaling, batch jobs for non-critical analytics, and elastic compute.
- Embed Observability from Launch: Monitor uptime, access patterns, and compliance metrics in real time.
- Plan for Continuous Improvement: Regularly update analytics models, security frameworks, and compliance modules.
Request a tailored proposal from Intellivon’s enterprise AI team, and you’ll receive a roadmap aligned with your budget, compliance obligations, and growth strategy, delivering a platform that is scalable, secure, and built to last.
Overcoming Challenges in Building a Patient Data Analytics Platform
Enterprises that embark on building patient data analytics platforms quickly discover that technology alone isn’t enough. The path is filled with challenges around security, compliance, integration, and adoption.
If left unresolved, these issues can slow down projects, inflate costs, or undermine trust. The good news is that with the right partner, every challenge can be turned into an opportunity for stronger systems and better outcomes.
1. Data Security and Privacy Risks
Healthcare data is a prime target for cyberattacks, and even a small breach can cost millions in penalties and reputational damage. Protecting sensitive patient information demands a full lifecycle approach covering ingestion, storage, access, and analytics.
Intellivon’s Approach: We embed encryption, de-identification, and continuous monitoring across every layer of the platform. By treating security as a living function rather than a checklist, we ensure that enterprises maintain control of patient data even in high-risk environments.
2. Integration with Legacy Systems
Many healthcare organizations still operate on legacy EHRs and billing systems that don’t follow modern interoperability standards. Without proper integration, data remains siloed, delaying insights and frustrating stakeholders who expect seamless access.
Intellivon’s Approach: We design secure middleware and use FHIR/HL7 APIs to connect old cores with modern cloud-native platforms. This ensures that legacy investments are protected while enabling fast, reliable data flows that power analytics without disruption.
3. Compliance with Multiple Regulations
HIPAA is only one piece of the puzzle. Global healthcare enterprises must also comply with GDPR, FDA guidance, and emerging regulations like the EU AI Act. Each introduces its own obligations around audit trails, data minimization, and patient rights.
Intellivon’s Approach: We build compliance into the architecture itself. Our frameworks align with HIPAA, GDPR, and FDA cybersecurity guidance from day one, so enterprises avoid costly retrofits. This compliance-first design allows organizations to expand confidently into new markets with audit-ready evidence.
4. High Implementation and Maintenance Costs
Healthcare leaders worry about hidden costs, such as middleware, compliance audits, and ongoing cloud usage, that can push projects over budget. Without careful planning, what starts as a strategic investment can quickly become unsustainable.
Intellivon’s Approach: We scope projects collaboratively, refine builds to fit budgets, and use modular components that scale with demand. Cloud-native optimization further reduces compute spend. The result is a predictable, transparent cost model that delivers value without unpleasant surprises.
Every challenge in building a patient data analytics platform can be reframed as an opportunity. Stronger security builds trust, interoperability fosters collaboration, and compliance creates a pathway for global expansion. By addressing these head-on, Intellivon helps enterprises move beyond obstacles and unlock the full potential of patient data analytics.
How We Make a Patient Data Analytics Platform Compliant
For healthcare enterprises, compliance is not negotiable. Patient data carries strict legal protections, and failing to meet them can lead to fines, lawsuits, and reputational damage that takes years to recover.
Building a compliant analytics platform demands a design that weaves regulatory standards into the very fabric of the system. At Intellivon, this is the principle behind every platform we deliver.
1. HIPAA Security Rule Safeguards
HIPAA is the baseline for protecting patient health information in the U.S. It requires risk analyses, encryption, access controls, and audit trails that prove accountability. Many organizations struggle to operationalize these requirements across fragmented systems.
We translate HIPAA safeguards into tangible design decisions, enforcing role-based access, encrypting data in motion and at rest, and embedding immutable logging. This makes compliance a built-in feature rather than a bolt-on afterthought.
2. GDPR and Global Privacy Requirements
For enterprises operating across borders, HIPAA alone is not enough. GDPR adds rules around consent, data minimization, and the right to be forgotten. These requirements demand transparency in how data is processed and stored.
We engineer governance frameworks that respect GDPR principles while still enabling advanced analytics. Data flows are documented, patient rights are protected, and opt-out mechanisms are automated. This ensures that platforms remain both globally scalable and locally compliant.
3. FDA and Medical Device Cybersecurity
When data comes from connected medical devices, additional regulations apply. The FDA requires proof that devices feeding into analytics systems are secure, updatable, and monitored for vulnerabilities. Many enterprises underestimate how this extends to their analytics infrastructure.
We validate device integrations against FDA cybersecurity guidance, require software bills of materials (SBOMs), and build secure update processes. By aligning analytics pipelines with device-level obligations, we close a common compliance gap.
4. ONC Interoperability and Audit-Readiness
The Office of the National Coordinator (ONC) mandates that systems support interoperability standards such as FHIR while maintaining auditability. This balance is often hard to achieve, and too much openness introduces risk, but too little hinders care delivery.
We secure FHIR and HL7 APIs with token-based access, scope restrictions, and anomaly detection. Every API call is logged, creating a transparent trail that satisfies ONC requirements while enabling safe data sharing across systems.
Compliance should not feel like a burden that slows innovation. When baked into architecture, it becomes a growth enabler, opening new markets, speeding up audits, and increasing patient trust.
At Intellivon, we design platforms that not only meet today’s HIPAA, GDPR, FDA, and ONC standards but are also flexible enough to adapt as regulations evolve. This future-proof approach ensures enterprises stay compliant, competitive, and trusted.
Future Trends in Patient Data Analytics Security
The security of patient data analytics platforms will not remain static. Regulations, technologies, and attack surfaces are evolving, and enterprises that fail to anticipate change will fall behind. Looking ahead, several trends will reshape how healthcare organizations protect and govern sensitive information.
1. AI-Powered Continuous Compliance
Traditional compliance audits happen annually or quarterly. Future platforms will embed AI systems that continuously assess compliance posture against HIPAA, GDPR, and new frameworks such as the EU AI Act.
Instead of waiting for an external audit, organizations will maintain a “live compliance scorecard,” with alerts triggered the moment a gap appears. This shift will make compliance proactive rather than reactive.
2. Zero-Knowledge Analytics
Enterprises will increasingly adopt zero-knowledge proofs in healthcare analytics. This cryptographic approach allows data to be analyzed without ever revealing the underlying patient details.
Hospitals could share outcome trends with payers or regulators without exposing individual PHI. For global enterprises, this will unlock new collaboration models where insights travel freely but raw data never leaves its secure environment.
3. Decentralized Identity and Access
Password-based access and even multi-factor authentication will give way to decentralized identity frameworks. These systems use blockchain-backed credentials to verify clinicians, researchers, and administrators without storing passwords or central tokens that can be stolen.
For patient analytics platforms, this will mean identity validation is distributed, tamper-proof, and scalable across geographies.
4. Federated Learning at Scale
Federated learning is still in its infancy, but in the coming years, it will become the standard for training healthcare AI models. Rather than centralizing sensitive patient data, models will learn across multiple institutions while keeping data local.
This will allow enterprises to build powerful predictive models across global populations without violating privacy regulations.
5. Real-Time Data Provenance Tracking
Future platforms will not only analyze data but also verify where it came from and how it was modified. Advances in blockchain and secure ledgers will allow enterprises to track every data point back to its origin.
This will reduce fraud, support clinical research integrity, and provide regulators with transparent, tamper-proof histories.
6. Security-Oriented AI Passports
Regulators in the U.S. and Europe are already exploring “AI passports” that certify models before deployment. In the near future, patient analytics platforms will embed these passports into their pipelines.
Every AI model will carry documentation of its training data, risk profile, and security status, ensuring enterprises deploy only compliant and auditable models.
7. Quantum-Resistant Encryption
The rise of quantum computing will render current encryption methods vulnerable. Forward-looking healthcare enterprises will adopt quantum-resistant encryption standards to protect patient data for decades.
Platforms that fail to modernize encryption will expose long-term records to retroactive attacks once quantum systems become mainstream.
These trends signal a fundamental shift that will make security an enabler of global collaboration, advanced analytics, and healthcare innovation. At Intellivon, we are already aligning our architectures with AI-driven compliance, federated learning, and decentralized identity so enterprises are prepared for the next decade of transformation.
Conclusion
Secure patient data analytics platforms are no longer optional—they are the backbone of modern healthcare enterprises. By embedding security, compliance, and resilience into every layer, these platforms reduce risk while unlocking the full value of healthcare data. They ensure decisions are faster, insights are reliable, and patient trust is preserved.
Looking forward, enterprises that invest in secure analytics today will be positioned to scale confidently into the future. With compliance baked in and security evolving alongside technology, these are enabling growth, innovation, and long-term sustainability in healthcare.
Build a Secure Patient Data Analytics Platform With Us
At Intellivon, we design patient data analytics platforms that are secure, compliant, and scalable. Each build aligns with the way modern healthcare enterprises operate, across clinical, operational, and financial workflows.
Our platforms combine privacy engineering, explainable analytics, and compliance-first architecture. You get real-time insight without compromising patient trust or regulatory confidence.
Why Partner With Intellivon?
- Tailored Enterprise Platforms: Every platform matches your operating model, data landscape, and compliance needs to deliver measurable ROI.
- Proven Healthcare Expertise: 11+ years, 500+ AI solutions, and 200+ domain experts solving complex healthcare challenges.
- Compliance-First Design: Built for HIPAA, GDPR, FDA cybersecurity guidance, and ONC interoperability requirements from day one.
- Future-Ready Architecture: Cloud-native, API-first, and designed to integrate with EHRs, LIMS, payers, and IoMT ecosystems.
- Security and Reliability: Multi-layered controls, immutable audit trails, and resilience patterns that keep services running during incidents.
- Interoperability at Scale: Hardened FHIR and HL7 gateways with scoped tokens, monitoring, and fine-grained access.
- Continuous Optimization and Support: Post-deployment tuning, governance updates, and model performance monitoring as regulations evolve.
- Transparent Value Tracking: Dashboards for adoption, uptime, and compliance readiness, so leadership sees progress in real time.
Book a free strategy call today to explore how Intellivon can help you build a secure, compliant patient data analytics platform that drives growth and trust.
FAQs
Q1. Why do hospitals need secure patient data analytics platforms?
A1. Hospitals handle vast amounts of sensitive health information, and unsecured systems expose them to breaches, penalties, and reputational damage. A secure analytics platform not only protects data but also enables faster, more accurate insights that improve patient care and operational efficiency.
Q2. How much does it cost to build a HIPAA-compliant patient data analytics system?
A2. Costs typically range between $50,000 and $150,000, depending on scope, integrations, and compliance requirements. Annual maintenance averages 15–20% of the initial build. Factors like legacy system integration, cloud usage, and regulatory updates also influence the total investment.
Q3. What are the best practices for API security in healthcare data platforms?
A3. Best practices include enforcing token-based authentication, limiting API permissions, encrypting traffic with TLS, and monitoring for abnormal requests. APIs should also be designed with scope restrictions to prevent unauthorized access to sensitive health records.
Q4. How do enterprises make patient data analytics GDPR and HIPAA compliant?
A4. Compliance requires embedding safeguards into the architecture. This includes encryption, de-identification, immutable audit logs, and role-based access. Enterprises must also align workflows with patient rights under GDPR and document every access point for HIPAA audits.
Q5. What is the ROI of building secure healthcare analytics platforms?
A5. ROI comes from avoided breach costs, reduced downtime, and faster audit cycles. Secure platforms also unlock predictive analytics that improve patient outcomes and streamline resource use. Together, these benefits create both financial savings and long-term trust.
Q6. How can hospitals reduce downtime with resilient analytics platforms?
A6. Resilient platforms are designed with failover systems, cached critical data, and real-time monitoring. If disruptions occur, the system shifts to backup environments with minimal interruption. This ensures that patient care and hospital operations continue without major impact.