Usually, physician performance reviews happen once a year, using data that is already more than six months old. Clinical leaders know which doctors are thriving and which are struggling, but that understanding comes from hallway chats and personal observations, not solid data. In the meantime, the organization holds terabytes of information, including patient outcomes, referral patterns, treatment costs, quality metrics, and patient satisfaction scores. The data is present, but what is not present is a system that makes it useful for clinicians.
The solution is physician performance analytics platforms, but not those that feel like surveillance tools. The effective platforms are built to provide doctors with context for their numbers instead of just rankings. Additionally, they also show areas for improvement along with successes and consider patient complexity and case mix. Most importantly, they are designed with input from physicians from the start.
At Intellivon, we have assisted healthcare organizations in creating these platforms for physician networks that include hundreds of providers. This blog discusses how we build these platforms from the ground up and how the right platform design can improve both clinical outcomes and organizational performance.
Why Physician Performance Analytics Platforms Matter
Performance analytics platforms bring together KPIs from operations, finance, sales, and workforce data into one unified system. As a result, leaders can make faster, evidence-based decisions instead of relying on fragmented reports.
Demand is rising quickly. Digital transformation initiatives are accelerating across industries. In addition, enterprises now expect AI-driven insights and real-time visibility into performance. Therefore, organizations are investing in platforms that turn raw data into actionable intelligence.
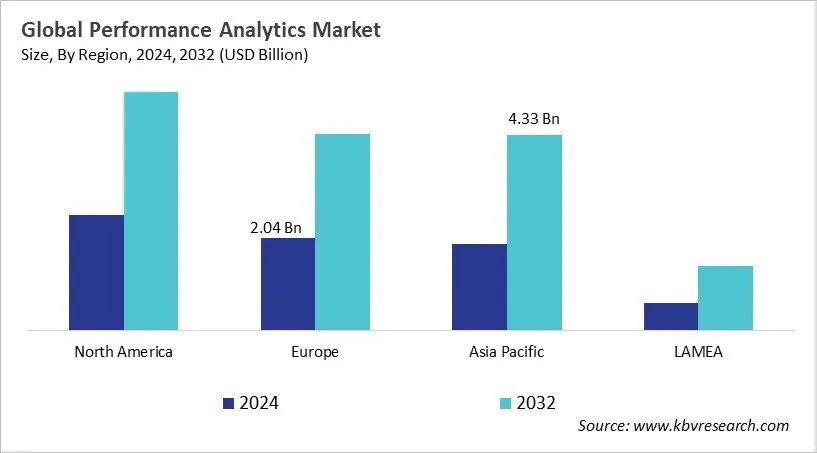
A recent report by KBV Research estimates that the global performance analytics market will reach $15.42 billion by 2032. The market is projected to grow at a compound annual growth rate of 10.3% during the forecast period.
This steady growth reflects rising enterprise demand for real-time insights, AI-driven decision support, and integrated performance visibility across business functions.
Market Growth Drivers:
- AI and machine learning enable predictive insights and anomaly detection. Therefore, enterprises improve efficiency and reduce operational risk.
- Cloud leads with a 55.4% market share. As a result, organizations gain scalability, cost savings, and secure remote access.
- Regulatory compliance and digital transformation drive adoption. BFSI holds 24.3% share, while healthcare and manufacturing continue expanding investments.
Why Healthcare Enterprises Are Using Physician Performance Analytics Platforms
Healthcare organizations are under sustained pressure to improve outcomes while controlling costs. At the same time, reimbursement models are evolving, and performance expectations are rising. Therefore, enterprises are investing in physician performance analytics platforms to bring structure, transparency, and accountability into clinical operations.
These platforms help leaders align care delivery with financial sustainability. In addition, they provide consistent visibility across specialties, facilities, and care teams. As a result, performance discussions move from anecdotal debate to data-backed decision-making.
1. Shift Toward Value-Based Care Models
Fee-for-service models are steadily giving way to value-based contracts. Under these arrangements, reimbursement depends on quality, efficiency, and measurable outcomes. Therefore, organizations need reliable performance intelligence to track readmissions, complication rates, and adherence to evidence-based protocols.
Without structured analytics, value-based participation becomes risky. With governed performance systems in place, however, leadership gains clarity on where improvements are required and where incentives align.
2. Demand for Transparent Performance Reporting
Clinical leaders increasingly expect visibility into how performance is measured. At the same time, executive teams require consistent reporting across departments. Therefore, physician analytics platforms centralize metrics and standardize definitions.
Transparency reduces internal friction. In addition, it supports more productive performance reviews and strategic planning conversations. When everyone sees the same numbers, alignment improves.
3. Linking Compensation to Measured Outcomes
Compensation models are evolving beyond pure productivity metrics. Many enterprises now blend RVUs with quality indicators, patient experience, and cost stewardship measures. As a result, compensation governance becomes more complex.
Physician performance analytics systems provide the structured data required to support incentive programs. They allow organizations to simulate thresholds, validate calculations, and ensure fairness before financial impact occurs.
4. Enterprise Need for Fair Performance Visibility
Fairness remains critical. Physicians must trust that comparisons account for case complexity and specialty differences. Therefore, advanced risk adjustment and peer benchmarking frameworks are essential.
When performance visibility is equitable and defensible, adoption improves. In turn, organizations strengthen accountability while maintaining clinical engagement and morale.
What Are Physician Performance Analytics Platforms?
Physician performance analytics platforms are centralized systems that track and measure how physicians perform across quality, productivity, cost, and patient experience. They combine data from EHRs, billing systems, registries, and scheduling tools into one structured environment. As a result, leaders gain a complete and consistent view of performance.
In practical terms, they answer critical questions:
- Are outcomes improving across specialties?
- Is productivity aligned with strategic goals?
- Are compensation models fair and defensible?
- Where does variation signal risk or opportunity?
In addition, physician performance analytics platforms reduce reliance on manual spreadsheets. They replace fragmented reporting with a controlled performance framework. Consequently, executives can align clinical quality, operational efficiency, and financial sustainability.
Ultimately, physician performance analytics platforms serve as a performance infrastructure. They bring structure to measurement, fairness to evaluation, and clarity to strategy.
Core Objectives of Physician Performance Analytics Platforms
Healthcare enterprises invest in physician performance analytics for clear, measurable reasons. These platforms are not built for reporting alone. Instead, they help organizations improve quality, control costs, and align incentives with long-term strategy.
When designed correctly, they support four core objectives.
1. Improve Clinical Quality and Patient Outcomes
First, organizations need reliable visibility into outcomes. Therefore, performance platforms track complication rates, readmissions, mortality trends, and adherence to clinical guidelines.
With structured analytics in place, variation becomes visible. In addition, quality teams can identify patterns across specialties and facilities. As a result, improvement initiatives become targeted rather than reactive.
Over time, this supports stronger patient outcomes and better value-based contract performance.
2. Enhance Operational Efficiency and Throughput
Second, enterprises must manage access and capacity. Physician analytics platforms track metrics such as length of stay, case turnaround time, clinic utilization, and panel size.
When leaders see workflow bottlenecks clearly, they can act faster. For example, they may adjust scheduling templates or redistribute workload across teams. Therefore, operational decisions become data-driven instead of assumption-based.
Efficiency gains often deliver impact within months.
3. Align Financial Performance With Enterprise Strategy
Clinical and financial performance are closely linked. However, without structured analytics, the connection remains unclear.
These platforms measure RVUs, cost per case, resource utilization, and contract alignment. In addition, they support the modeling of incentive programs tied to quality and efficiency.
As a result, financial governance becomes more stable. Compensation decisions rely on validated data rather than isolated calculations.
4. Create Fair and Transparent Performance Visibility
Finally, fairness drives adoption. Physicians must trust that performance comparisons account for case complexity and specialty differences.
Therefore, physician performance analytics platforms apply risk adjustment and peer benchmarking. They also allow drilldown access to underlying data.
When visibility is transparent and defensible, engagement improves. In turn, performance discussions shift from dispute to improvement.
In summary, the core objectives extend beyond measurement. These platforms improve quality, strengthen operations, protect financial stability, and support a sustainable performance culture.
Architecture for Physician Performance Analytics Platforms
Data architecture for physician performance analytics platforms integrates EHR, billing, registry, and operational data into a governed, risk-adjusted framework that ensures accurate, audit-ready performance measurement.
Strong physician performance analytics begins with strong data architecture. Without a structured foundation, even the best dashboards fail. Therefore, enterprises must design the platform as core infrastructure, not an add-on reporting tool.
The goal is to bring clinical, operational, and financial data into one governed environment. After that, the goal is to then apply consistent logic to calculate metrics accurately and transparently. Below are the essential components:
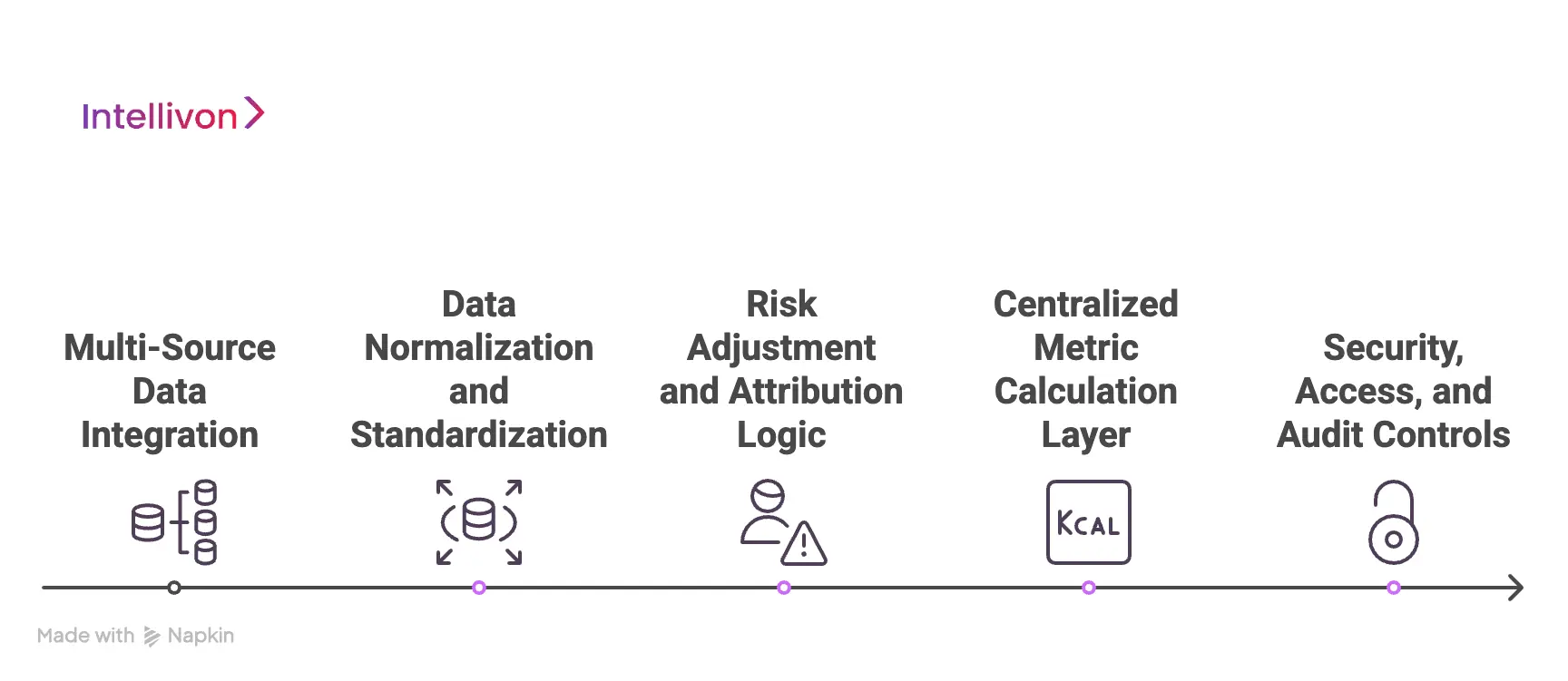
1. Multi-Source Data Integration
Physician performance depends on multiple systems. EHR data captures clinical outcomes. Billing systems track productivity and revenue. Quality registries provide benchmarking inputs. Scheduling systems reveal access and capacity trends.
These data streams must connect through secure pipelines. In addition, integration should occur at the encounter and episode level. When data flows remain fragmented, metrics become inconsistent. Therefore, centralized ingestion is critical.
2. Data Normalization and Standardization
Raw data cannot drive fair comparisons. Coding structures differ across departments and facilities. Therefore, the platform must harmonize CPT, ICD, DRG, and internal coding standards.
Standardization ensures that one procedure means the same thing across the enterprise. In addition, it reduces calculation errors that erode trust. Clean data is not optional. It is foundational.
3. Risk Adjustment and Attribution Logic
Performance comparisons must account for case complexity. Therefore, the architecture should embed risk adjustment models and attribution rules within the calculation layer.
For example, a tertiary referral center may treat more complex cases. Without normalization, metrics appear distorted. In addition, clear attribution rules ensure that responsibility aligns with actual clinical involvement. When this logic is transparent and version-controlled, credibility increases.
4. Centralized Metric Calculation Layer
Every KPI should be calculated in one controlled environment. If departments calculate metrics separately, discrepancies emerge quickly.
A centralized logic engine prevents fragmentation. It also allows updates to metric definitions without disrupting historical reporting. As a result, the organization maintains consistency over time.
5. Security, Access, and Audit Controls
Performance data is sensitive. Therefore, role-based access controls must limit visibility appropriately. Here, individual physicians should see their own data, service line leaders should view peer comparisons, and enterprise leaders should access aggregated trends.
In addition, audit trails should track metric changes and data updates. This protects the organization during compliance reviews and compensation validation processes.
In summary, data architecture determines the credibility of physician performance analytics platforms. When integration, standardization, risk adjustment, and governance work together, performance measurement becomes reliable. Consequently, leadership can act with confidence rather than hesitation.
Risk Adjustment Strategy for Physician Performance Analytics Platforms
Risk adjustment in physician performance analytics platforms ensures fair comparisons by accounting for case complexity, comorbidities, referral patterns, and patient demographics before evaluating outcomes or productivity.
At the same time, risk adjustment determines whether physician performance analytics feels fair or flawed. Without it, high-acuity providers appear inefficient. In contrast, low-complexity practices may look artificially strong. Therefore, enterprises must treat risk modeling as core infrastructure.
A strong risk adjustment strategy protects trust. At the same time, it also protects the organization from flawed compensation decisions and contract misalignment. Below are the essential elements:
1. Why Risk Adjustment Matters
Physicians do not treat identical patients. At the same time, case severity, referral patterns, and population health profiles vary widely. Therefore, raw metrics distort reality.
For example:
- A tertiary hospital manages complex surgical cases.
- A community clinic treats routine, lower-risk patients.
- An oncology team handles high-morbidity populations.
- A primary care panel may include a significant chronic disease burden.
If outcomes are compared without normalization, conclusions become misleading. As a result, performance discussions turn defensive instead of constructive.
2. Core Components of a Risk Adjustment Strategy
Effective physician performance analytics platforms apply structured normalization across several dimensions.
A. Clinical Severity Adjustment
Models should incorporate:
- Comorbidity indexes
- Disease staging
- Procedural risk categories
- Emergency versus elective classification
This ensures complication rates reflect true case difficulty.
B. Case-Mix Index Normalization
The case-mix index helps adjust financial and operational metrics. Therefore, cost per case and length of stay comparisons remain grounded in complexity.
C. Specialty-Specific Modeling
Risk models must reflect the specialty context. Cardiology metrics differ from orthopedic benchmarks. In addition, oncology requires longitudinal outcome tracking. At the same time, generic scoring frameworks rarely work across all disciplines.
D. Socioeconomic and Population Factors
Readmission rates and adherence outcomes often correlate with social determinants. Therefore, patient demographics and access factors may require adjustment.
Ignoring these variables can penalize providers serving vulnerable populations.
3. Addressing Referral and Tertiary Bias
Referral centers often manage more advanced cases. Consequently, mortality or complication rates may appear elevated without proper correction.
A mature risk adjustment strategy should:
- Identify referral patterns
- Segment elective versus transfer cases
- Normalize outcomes for tertiary exposure
When this logic is transparent, confidence improves.
4. Managing Small Sample Volatility
Performance metrics fluctuate when sample sizes are small. Therefore, statistical smoothing techniques help stabilize reporting.
Common approaches include:
- Rolling averages across quarters
- Minimum case thresholds before scoring
- Confidence interval reporting
These controls prevent overreaction to short-term variance.
5. Governance and Model Transparency
Risk models must be documented and version-controlled. In addition, changes should be reviewed by a clinical governance council.
Enterprises should clearly define:
- Which variables influence each metric
- How updates are approved
- How historical data remains comparable
When physicians understand the methodology, adoption increases. When logic remains hidden, skepticism grows.
In summary, risk adjustment is not a technical detail. It is the foundation of fair physician performance analytics. When properly designed, it enables credible benchmarking, stable compensation governance, and strategic decision-making. Therefore, organizations that invest in structured risk modeling build stronger performance cultures over time.
Advanced Features Of Physician Performance Analytics Platforms
Advanced physician performance analytics platforms use predictive modeling, AI-driven insights, and behavioral analytics to detect risk early, reduce variation, and support value-based enterprise strategy.
Therefore, these features directly support strategic planning and contract readiness. Below are the capabilities that separate mature platforms from basic reporting systems.
1. Predictive Quality Risk Modeling
Traditional dashboards show what has already happened. Predictive modeling estimates what is likely to happen next.
For example, platforms can identify:
- Patients at high risk of readmission
- Surgeons trending toward complication thresholds
- Service lines approaching quality contract penalties
By analyzing historical patterns and current inputs, the system flags early warnings. As a result, leadership can intervene before metrics deteriorate.
This approach strengthens value-based contract performance and protects reputation.
2. Real-Time Outlier Detection
Outlier detection identifies unusual performance patterns in near real time. Instead of waiting for quarterly reviews, the platform continuously monitors deviation from expected ranges.
It can surface:
- Unexpected cost spikes per procedure
- Sudden shifts in documentation behavior
- Abnormal length-of-stay patterns
However, the system must distinguish statistical noise from meaningful change. Therefore, outlier logic should incorporate confidence intervals and minimum volume thresholds.
When implemented correctly, real-time alerts improve responsiveness without creating unnecessary alarms.
3. Compensation and Incentive Simulation
Advanced platforms allow organizations to model compensation changes before activation. This prevents financial misalignment and internal disruption.
Simulation tools can test:
- Bonus threshold adjustments
- Blended RVU and quality weighting models
- Shared savings distribution scenarios
- Sensitivity to case-mix fluctuations
Instead of reacting to unexpected payout outcomes, enterprises validate impact beforehand. Consequently, compensation governance becomes more stable and predictable.
4. Burnout and Workforce Risk Indicators
Workforce sustainability now sits alongside financial and quality priorities. Physician performance analytics platforms can analyze workload patterns to detect strain.
Signals may include:
- Excessive after-hours documentation
- Disproportionate patient panel size
- High case complexity concentration
- Declining productivity with rising administrative load
These insights do not label individuals. Instead, they highlight systemic imbalance. Therefore, leadership can adjust staffing models or workflow design before attrition rises.
5. Referral and Network Pattern Analysis
In large health systems, referral behavior influences revenue and care continuity. Advanced analytics can map referral flows across specialties and facilities.
This reveals:
- Leakage outside the network
- Over-concentration of cases within certain teams
Gaps in service access
As a result, strategic planning becomes data-driven. Growth initiatives align with actual utilization patterns rather than assumptions.
6. Longitudinal Performance Stability Monitoring
Performance should not fluctuate wildly due to small sample sizes. Advanced platforms apply smoothing techniques and trend analysis across time.
They can:
- Compare rolling quarterly averages
- Detect gradual improvement or decline
- Highlight sustained variation instead of short-term noise
Therefore, leadership focuses on durable trends instead of isolated spikes.
Advanced capabilities elevate physician performance analytics from reporting infrastructure to a strategic command center. They allow enterprises to anticipate risk, refine incentives, protect workforce stability, and optimize network performance.
When predictive insights and governance operate together, organizations move from reactive correction to proactive strategy. Over time, this shift strengthens quality, financial resilience, and enterprise growth.
How We Build Physician Performance Analytics Platforms
At Intellivon, we build physician performance analytics platforms as an enterprise healthcare performance infrastructure. That means we prioritize accuracy, governance, and long-term stability from day one. As a result, organizations avoid the common trap of launching dashboards that teams do not trust.
Below is our step-by-step build approach. Each step is designed to deliver value early, while keeping the platform defensible at scale.
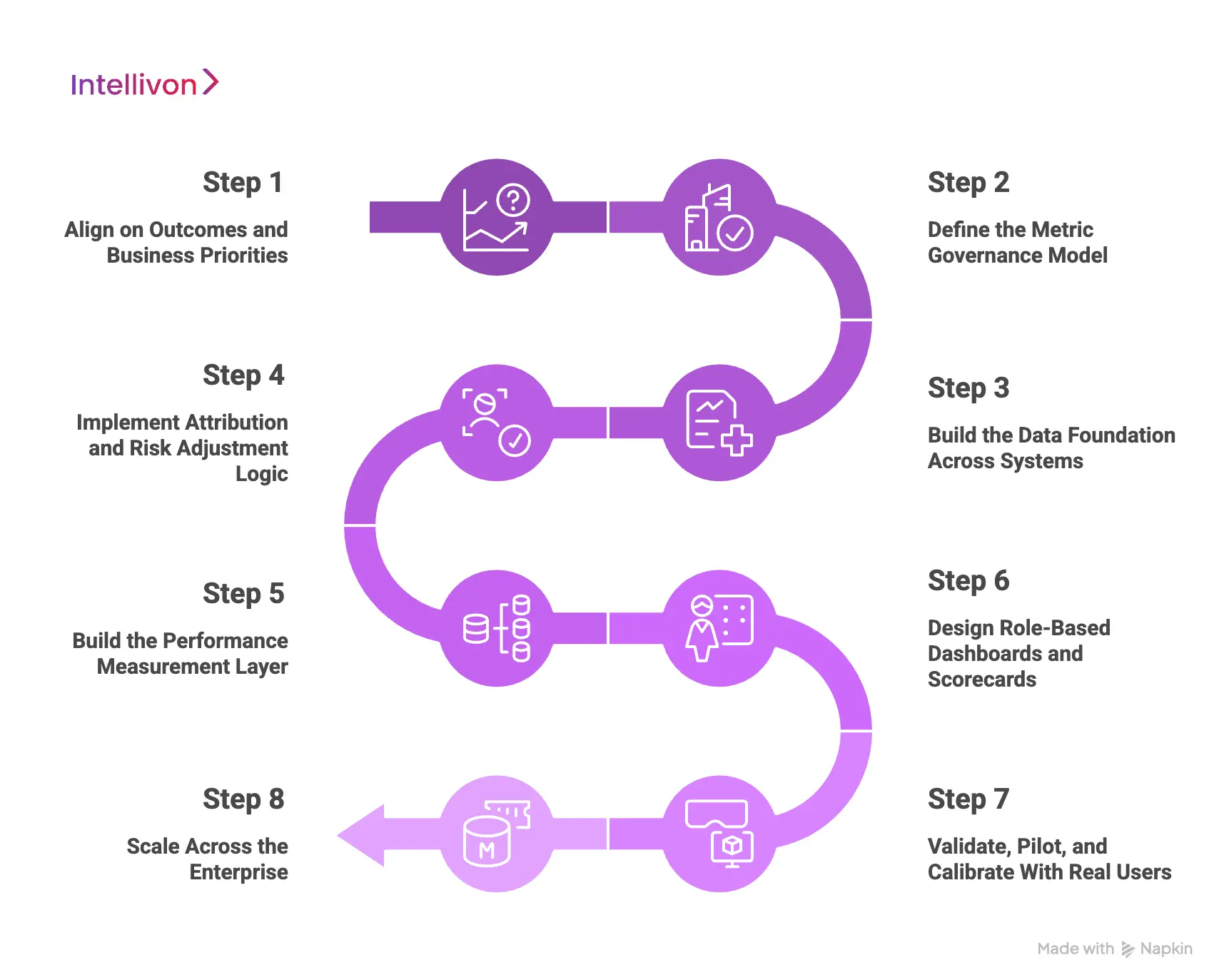
Step 1: Align on Outcomes and Business Priorities
We start by clarifying what the enterprise needs to improve. Therefore, we map performance goals to measurable outcomes.
This typically includes:
- Quality outcomes tied to contracts and safety goals
- Access and throughput constraints impacting growth
- Cost variation and resource stewardship targets
- Compensation governance and incentive design needs
In addition, we define success criteria upfront. This keeps the platform focused and prevents metric sprawl.
Step 2: Define the Metric Governance Model
Next, we set governance before we build dashboards. This ensures consistency across facilities, specialties, and reporting cycles.
We establish:
- Standard metric definitions and calculation rules
- Ownership for each metric domain
- Review workflows for changes and exceptions
- Audit trails for metric versioning and updates
As a result, leadership gains control. Physicians also gain clarity.
Step 3: Build the Data Foundation Across Systems
We then integrate the systems that drive physician performance measurement. Therefore, the platform connects to clinical, operational, and financial sources.
Common inputs include:
- EHR clinical and encounter data
- Billing, claims, and coding data
- Quality registries and benchmarking feeds
- Scheduling, access, and capacity data
In addition, we normalize coding and terminology. This improves comparability across sites.
Step 4: Implement Attribution and Risk Adjustment Logic
This step protects fairness. Without it, performance scores lose credibility quickly.
We implement:
- Encounter and episode attribution rules
- Multi-provider contribution logic where needed
- Specialty-aware risk adjustment models
- Case-mix normalization for cost and throughput metrics
Therefore, comparisons reflect real clinical complexity, not raw averages.
Step 5: Build the Performance Measurement Layer
After the logic is stable, we create the KPI calculation engine. This is the layer that produces consistent performance metrics.
We focus on:
- Centralized metric computation
- Controlled refresh cycles and data validation
- Historical snapshots for trend accuracy
- Reliable drilldowns to encounter-level detail
As a result, performance conversations rely on the same source of truth.
Step 6: Design Role-Based Dashboards and Scorecards
Now we build the experience layer. However, we keep it structured and purposeful.
We deliver:
- Enterprise views for network performance trends
- Service line dashboards for operational ownership
- Physician-level scorecards with drilldowns
- Exception views for quality and compliance teams
In addition, we apply role-based access control. This protects privacy while supporting transparency.
Step 7: Validate, Pilot, and Calibrate With Real Users
We do not treat launch as the finish line. Instead, we pilot with selected specialties and refine the platform based on reality.
During the pilot, we ran:
- Metric validation sessions with clinical leaders
- Data quality and attribution audits
- Usability testing for drilldowns and workflows
- Feedback-driven refinements to benchmarks and thresholds
Therefore, adoption grows because the platform feels accurate and fair.
Step 8: Scale Across the Enterprise
We support:
- Ongoing metric lifecycle management
- New specialty onboarding and benchmarking updates
- Value-based contract alignment and reporting readiness
- Advanced capabilities such as predictive risk signals
As a result, the platform evolves without losing consistency.
Physician performance analytics platforms succeed when they are governed, risk-adjusted, and built for enterprise adoption. That is how Intellivon delivers durable performance infrastructure, not short-term reporting.
If you want to build a physician performance analytics platform that leaders can rely on and physicians can trust, Intellivon can help you design and deliver it end-to-end.
Building Physician Trust in Performance Analytics Platforms
Physician trust in performance analytics platforms increases when metrics are transparent, risk-adjusted, auditable, and supported by clear governance and dispute resolution workflows.
Even the most advanced physician performance analytics platform will fail without trust. Physicians must believe that the data is accurate, the comparisons are fair, and the intent is constructive. Therefore, trust must be designed into the system from the start.
When trust exists, performance conversations become collaborative. However, when transparency is missing, resistance builds quickly. As a result, adoption slows, and shadow reporting begins. Below are the pillars of trust-driven implementation:
1. Transparent Metric Definitions
Physicians should never guess how a score is calculated. Every metric must have a clear definition, data source, and calculation logic.
This includes:
- Exact numerator and denominator logic
- Risk adjustment variables used
- Attribution rules applied
- Reporting frequency and update cycle
When definitions are accessible, skepticism declines. In addition, transparency reduces unnecessary disputes during reviews.
2. Access to Underlying Encounter Data
Aggregated scores alone create frustration. Physicians need the ability to drill down into specific cases.
Therefore, platforms should allow:
- Encounter-level detail views
- Timeline-based performance trends
- Case filters by diagnosis or procedure
- Clear flags for data anomalies
This visibility shifts the conversation from abstract scoring to actionable insight.
3. Fair Peer Benchmarking
Comparisons should reflect specialty, case complexity, and practice setting. For example, a high-acuity surgeon should not be compared with a routine outpatient provider.
Effective benchmarking includes:
- Specialty-aligned peer groups
- Case-mix normalization
- Volume-adjusted scoring thresholds
When peers are appropriately matched, performance reviews feel balanced rather than punitive.
4. Structured Dispute and Review Process
Even with strong data architecture, discrepancies can occur. Therefore, organizations need a formal review workflow.
A mature process should include:
- Clear submission pathway for metric review
- Defined turnaround timelines
- Clinical leadership oversight
- Documented resolution outcomes
This structure demonstrates that leadership values fairness over speed.
5. Gradual Rollout and Early Engagement
Trust does not build overnight. Enterprises should begin with controlled pilots across select specialties. During this phase, feedback loops remain active.
Leaders should:
- Conduct walkthrough sessions
- Invite clinical input on metric refinement
- Adjust models based on practical insight
Early collaboration strengthens long-term adoption.
Physician performance analytics platforms succeed when they are seen as improvement tools rather than evaluation mechanisms. Trust emerges from transparency, fairness, and governance.
When physicians understand the data and influence the process, engagement increases. In turn, performance discussions focus on quality and outcomes rather than defensive debate.
Ultimately, trust transforms analytics from a reporting system into a shared performance framework.
Conclusion
Physician performance analytics is becoming essential for healthcare enterprises. When built with strong governance, fair risk adjustment, and clear attribution, it strengthens quality, financial stability, and operational control. More importantly, it builds physician trust and supports long-term growth.
Organizations that treat performance analytics as core infrastructure, not reporting add-ons, position themselves to compete effectively in value-based and outcome-driven care environments.
Build A Physician Performance Analytics Platform With Intellivon
At Intellivon, physician performance analytics platforms are built as a regulated healthcare performance infrastructure, not as reporting dashboards layered onto EHR systems. Every architectural and delivery decision prioritizes governance, risk adjustment, integrity, attribution accuracy, and audit readiness. This ensures performance measurement remains fair, defensible, and stable across specialties, facilities, and care networks.
As organizations expand value-based contracts and compensation models, performance visibility becomes more complex. Therefore, stability, transparency, and compliance must scale with volume and complexity. Intellivon platforms maintain consistent metric logic, controlled updates, and secure access as data sources grow. Enterprises retain control over definitions, benchmarks, and incentive alignment without introducing fragmentation or internal disputes.
Why Partner With Intellivon?
- Enterprise-grade performance architecture built for regulated healthcare environments
- Proven experience designing governed, risk-adjusted physician analytics frameworks
- Attribution modeling that supports fair benchmarking across specialties
- Compliance-by-design with audit trails and defensible metric lifecycle control
- Secure, modular infrastructure for cloud, hybrid, and on-prem deployment
- AI-enabled predictive insights with built-in oversight and governance
Book a strategy call to explore how Intellivon can help you design and scale a physician performance analytics platform with fairness, stability, and long-term enterprise impact.
FAQ’s
Q1. What is physician performance analytics?
A1. Physician performance analytics refers to systems that measure clinical quality, productivity, cost, and patient experience at the provider level. These platforms combine EHR, billing, and operational data into structured dashboards. As a result, healthcare enterprises can evaluate performance fairly and consistently across specialties and facilities.
Q2. How do hospitals measure physician performance fairly?
A2. Hospitals measure physician performance using risk-adjusted metrics and specialty-specific benchmarks. They normalize for case complexity, patient demographics, and referral patterns. In addition, they apply clear attribution rules to assign responsibility accurately. Therefore, comparisons remain balanced and defensible.
Q3. Why is risk adjustment important in physician analytics?
A3. Risk adjustment ensures that physicians treating complex patients are not penalized unfairly. Without normalization, raw outcome metrics can misrepresent performance. Consequently, trust declines. When risk models are transparent and specialty-aware, benchmarking becomes credible and adoption improves.
Q4. How do physician performance analytics platforms support value-based care?
A4. These platforms track quality measures, cost variation, and outcome trends tied to contracts. They help organizations monitor readmissions, complications, and utilization patterns. As a result, leadership can intervene early and protect reimbursement under value-based payment models.
Q5. Can physician performance analytics improve operational efficiency?
A5. Yes. Performance analytics highlights workflow bottlenecks, documentation delays, and throughput variation. In addition, it identifies productivity trends and panel imbalances. Therefore, healthcare enterprises can adjust staffing, scheduling, and care pathways to improve efficiency without compromising quality.